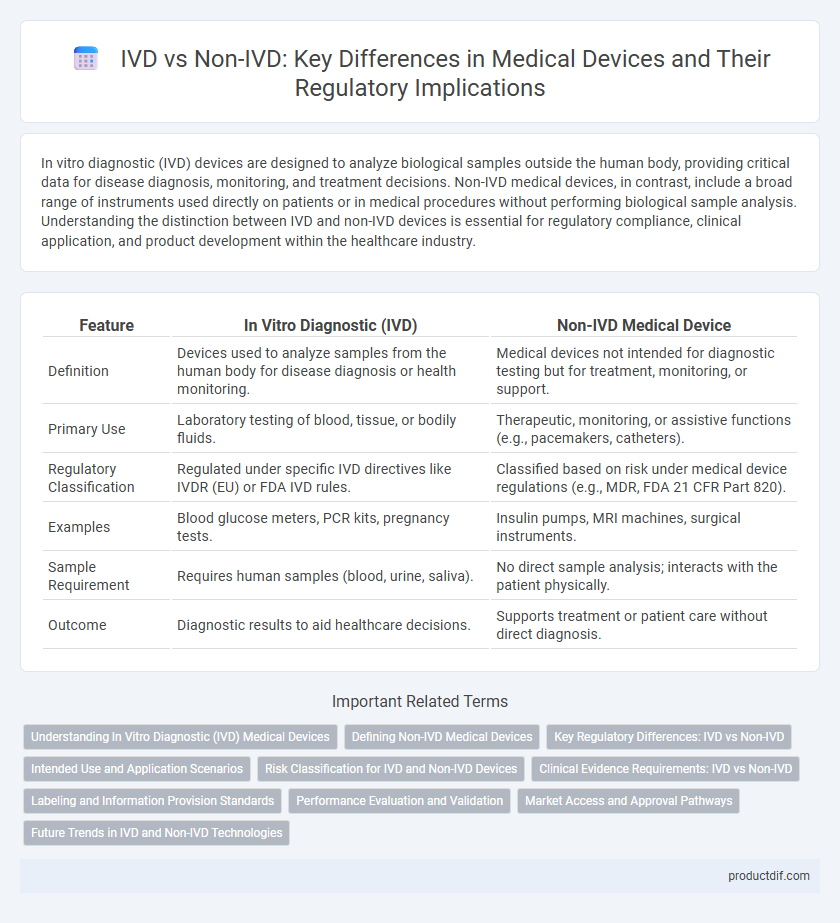
In vitro diagnostic (IVD) devices are designed to analyze biological samples outside the human body, providing critical data for disease diagnosis, monitoring, and treatment decisions. Non-IVD medical devices, in contrast, include a broad range of instruments used directly on patients or in medical procedures without performing biological sample analysis. Understanding the distinction between IVD and non-IVD devices is essential for regulatory compliance, clinical application, and product development within the healthcare industry.
Table of Comparison
| Feature | In Vitro Diagnostic (IVD) | Non-IVD Medical Device |
|---|---|---|
| Definition | Devices used to analyze samples from the human body for disease diagnosis or health monitoring. | Medical devices not intended for diagnostic testing but for treatment, monitoring, or support. |
| Primary Use | Laboratory testing of blood, tissue, or bodily fluids. | Therapeutic, monitoring, or assistive functions (e.g., pacemakers, catheters). |
| Regulatory Classification | Regulated under specific IVD directives like IVDR (EU) or FDA IVD rules. | Classified based on risk under medical device regulations (e.g., MDR, FDA 21 CFR Part 820). |
| Examples | Blood glucose meters, PCR kits, pregnancy tests. | Insulin pumps, MRI machines, surgical instruments. |
| Sample Requirement | Requires human samples (blood, urine, saliva). | No direct sample analysis; interacts with the patient physically. |
| Outcome | Diagnostic results to aid healthcare decisions. | Supports treatment or patient care without direct diagnosis. |
Understanding In Vitro Diagnostic (IVD) Medical Devices
In vitro diagnostic (IVD) medical devices are designed to analyze biological samples outside the human body, providing critical information for disease diagnosis, monitoring, and treatment decisions. Unlike non-IVD devices, which may serve therapeutic or monitoring functions without direct sample analysis, IVDs include instruments like blood glucose meters, pregnancy tests, and molecular diagnostic tools. Regulatory frameworks for IVDs emphasize accuracy, reliability, and patient safety due to their direct impact on clinical outcomes and public health.
Defining Non-IVD Medical Devices
Non-IVD medical devices refer to instruments, apparatuses, or machines used for medical purposes that do not perform diagnostic testing on biological samples. These devices include surgical instruments, pacemakers, imaging equipment, and implants designed to treat, monitor, or support patients without analyzing specimens like blood or tissue. In contrast to in vitro diagnostics, Non-IVD devices primarily focus on therapeutic, monitoring, or surgical functions rather than diagnostic analysis.
Key Regulatory Differences: IVD vs Non-IVD
In vitro diagnostic (IVD) devices are subject to stringent regulatory frameworks such as the FDA's 21 CFR Part 809 and the EU's IVDR, which require comprehensive performance evaluations and risk management specific to diagnostic accuracy. Non-IVD medical devices typically follow general medical device regulations like FDA's 21 CFR Part 820 and EU MDR, emphasizing safety and efficacy without the need for diagnostic performance validation. Key regulatory differences include the classification systems, premarket submission requirements, and post-market surveillance protocols tailored to the inherent risks and purposes of IVD versus non-IVD devices.
Intended Use and Application Scenarios
In vitro diagnostic (IVD) devices are specifically intended for the examination of specimens derived from the human body to detect diseases, conditions, or infections, enabling clinical decision-making and patient management. Non-IVD medical devices, by contrast, are designed for purposes other than diagnostic testing, such as therapeutic intervention, monitoring, or support, and are typically used directly on or in the body without specimen analysis. The distinct application scenarios of IVDs involve laboratory or point-of-care testing environments, while Non-IVD devices are applied in surgical, therapeutic, or monitoring settings.
Risk Classification for IVD and Non-IVD Devices
In vitro diagnostic (IVD) devices are classified based on risk categories ranging from Class A (low risk) to Class D (high risk), reflecting their potential impact on patient health and public safety. Non-IVD medical devices follow a separate risk classification system, typically categorized from Class I to Class III, with Class III indicating the highest risk due to invasive use or critical function. Understanding these risk classifications is essential for regulatory compliance, ensuring appropriate safety measures and clinical efficacy for both IVD and Non-IVD devices.
Clinical Evidence Requirements: IVD vs Non-IVD
Clinical evidence requirements for In Vitro Diagnostics (IVD) are more stringent compared to Non-IVitro Diagnostic (Non-IVD) devices due to direct impact on patient diagnosis and treatment decisions. IVD manufacturers must provide robust analytical and clinical performance data, including sensitivity, specificity, and reproducibility, validated through clinical studies. Non-IVD devices generally rely on performance testing and literature to demonstrate safety and effectiveness, with less emphasis on extensive clinical trials.
Labeling and Information Provision Standards
In vitro diagnostic (IVD) medical devices require stringent labeling and information provision standards to ensure accurate interpretation of test results and patient safety. IVD labeling must include detailed instructions for use, specimen collection guidelines, and interpretation criteria compliant with regulatory frameworks such as the FDA and IVDR. Non-IVD devices generally follow less rigorous labeling standards, focusing primarily on device operation and safety warnings without the critical diagnostic specificity mandated for IVD products.
Performance Evaluation and Validation
Performance evaluation and validation of in vitro diagnostic (IVD) devices involve rigorous analytical and clinical assessments to ensure accuracy, sensitivity, and specificity in detecting biomarkers or pathogens. Non-IVD devices undergo performance testing primarily focused on mechanical reliability and safety rather than diagnostic accuracy, reflecting their broader functional roles. Compliance with regulatory standards such as ISO 13485 and FDA 21 CFR Part 820 is critical for both categories, though the depth and nature of validation differ significantly based on intended use.
Market Access and Approval Pathways
In vitro diagnostic (IVD) devices undergo stringent regulatory approval processes, often requiring extensive clinical data to demonstrate safety and efficacy, facilitating market access primarily through regulatory bodies such as the FDA in the U.S. and the European Medicines Agency (EMA) in Europe. Non-IVD medical devices typically follow different classification systems and may have faster or less rigorous approval pathways, depending on the risk class and intended use, allowing for variable market entry timelines. Understanding these distinct regulatory frameworks is crucial for strategic planning in medical device commercialization and ensuring compliance with region-specific market access requirements.
Future Trends in IVD and Non-IVD Technologies
Future trends in in vitro diagnostic (IVD) technologies emphasize advancements in molecular diagnostics, point-of-care testing, and integration with artificial intelligence to enable faster, more accurate disease detection. Non-IVD medical devices are evolving through wearable sensors and implantable systems that provide continuous patient monitoring and real-time health data analytics. The convergence of digital health platforms with IVD and non-IVD tools is driving personalized medicine, improving treatment outcomes and healthcare efficiency.
In vitro diagnostic (IVD) vs Non-IVD Infographic
 productdif.com
productdif.com