Orthopedic implants are designed to support and replace damaged bones or joints in the musculoskeletal system, often made from materials like titanium or stainless steel for durability and biocompatibility. Dental implants primarily replace missing teeth and are typically crafted from titanium, integrating with jawbone through osseointegration to provide a stable foundation for crowns or bridges. Both implant types require precise surgical placement and focus on restoring function, but differ significantly in their anatomical application and biomechanical requirements.
Table of Comparison
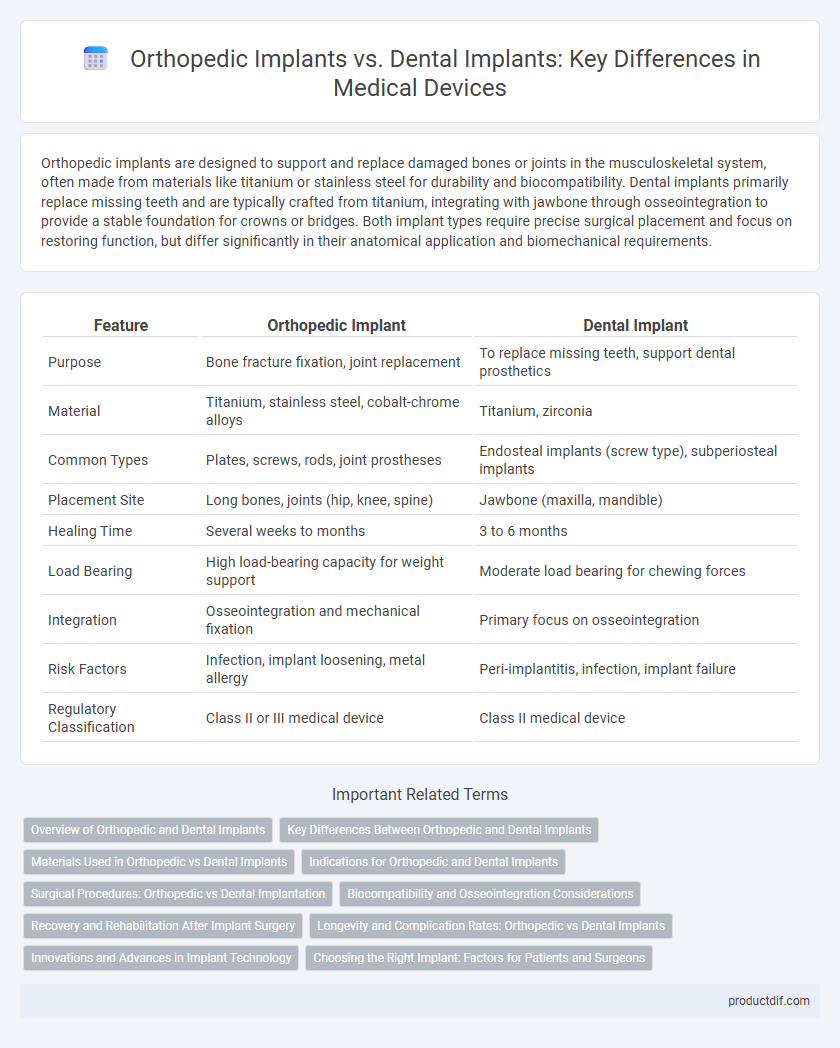
| Feature | Orthopedic Implant | Dental Implant |
|---|---|---|
| Purpose | Bone fracture fixation, joint replacement | To replace missing teeth, support dental prosthetics |
| Material | Titanium, stainless steel, cobalt-chrome alloys | Titanium, zirconia |
| Common Types | Plates, screws, rods, joint prostheses | Endosteal implants (screw type), subperiosteal implants |
| Placement Site | Long bones, joints (hip, knee, spine) | Jawbone (maxilla, mandible) |
| Healing Time | Several weeks to months | 3 to 6 months |
| Load Bearing | High load-bearing capacity for weight support | Moderate load bearing for chewing forces |
| Integration | Osseointegration and mechanical fixation | Primary focus on osseointegration |
| Risk Factors | Infection, implant loosening, metal allergy | Peri-implantitis, infection, implant failure |
| Regulatory Classification | Class II or III medical device | Class II medical device |
Overview of Orthopedic and Dental Implants
Orthopedic implants, such as joint replacements and bone plates, are designed to support or replace damaged bones and joints, promoting mobility and structural integrity. Dental implants serve as artificial tooth roots, typically made of titanium, anchored into the jawbone to support crowns, bridges, or dentures for tooth restoration. Both implant types require biocompatible materials and precise surgical techniques to ensure integration with natural bone and long-term stability.
Key Differences Between Orthopedic and Dental Implants
Orthopedic implants are designed to support or replace bones and joints, such as hip or knee replacements, focusing on load-bearing and structural stability within the musculoskeletal system. Dental implants serve as artificial tooth roots anchoring prosthetic teeth, prioritizing osseointegration with the jawbone and restoration of oral function. Material composition differs, with orthopedic implants often made from titanium alloys or stainless steel for strength, while dental implants typically use pure titanium or zirconia for biocompatibility and aesthetic integration.
Materials Used in Orthopedic vs Dental Implants
Orthopedic implants primarily utilize biocompatible metals such as titanium alloys, stainless steel, and cobalt-chromium for their strength and durability in load-bearing applications. Dental implants often employ titanium and zirconia, chosen for their exceptional osseointegration properties and aesthetic compatibility with natural teeth. Material selection in orthopedic versus dental implants is driven by differing functional demands, with orthopedic requiring enhanced mechanical performance and dental prioritizing biocompatibility and appearance.
Indications for Orthopedic and Dental Implants
Orthopedic implants are primarily indicated for the stabilization and repair of bone fractures, joint replacements, and spinal decompression, addressing conditions such as osteoarthritis, traumatic injuries, and degenerative bone disorders. Dental implants are used to replace missing teeth, support dental prosthetics, and restore oral function and aesthetics, typically indicated for patients with tooth loss due to decay, periodontal disease, or trauma. Both implant types require precise surgical planning and patient-specific considerations to ensure successful integration and long-term functionality.
Surgical Procedures: Orthopedic vs Dental Implantation
Orthopedic implant surgical procedures often involve extensive bone preparation, including drilling and reaming to accommodate large implants designed for load-bearing functions. Dental implant surgery typically requires precise, minimally invasive techniques to place smaller titanium fixtures into the jawbone, promoting osseointegration for tooth replacement. Both procedures demand sterile environments and postoperative care to ensure successful integration and prevent infection.
Biocompatibility and Osseointegration Considerations
Orthopedic implants and dental implants both require excellent biocompatibility to minimize immune response and ensure tissue acceptance, but dental implants face stricter demands due to the oral environment's exposure to saliva and microbial flora. Osseointegration is critical for both, with titanium and titanium alloys commonly used in orthopedic implants to promote bone integration, while dental implants often utilize surface modifications like hydroxyapatite coatings to enhance bonding with the jawbone. Differences in mechanical load and anatomical site influence material choice and design, optimizing long-term stability and functionality in each implant type.
Recovery and Rehabilitation After Implant Surgery
Recovery after orthopedic implant surgery typically involves a longer rehabilitation period focusing on regaining mobility, strength, and joint function through physical therapy. Dental implant recovery is generally faster, emphasizing osseointegration, where the implant fuses with the jawbone, and patients can resume normal oral functions within weeks. Rehabilitation protocols for orthopedic implants are more intensive due to the complexity of bone and joint structures, whereas dental implants require less invasive post-operative care.
Longevity and Complication Rates: Orthopedic vs Dental Implants
Orthopedic implants typically exhibit greater longevity due to the use of durable materials like titanium alloys and cobalt-chromium, which support weight-bearing functions over decades with complication rates such as infection and implant loosening ranging between 1-5%. Dental implants, primarily composed of titanium or zirconia, show high success rates exceeding 95% over 10-15 years, but complications like peri-implantitis and osseointegration failure occur in approximately 5-10% of cases. Both implant types demand rigorous surgical technique and postoperative care to minimize risks and maximize functional lifespan.
Innovations and Advances in Implant Technology
Orthopedic implants have seen innovations such as bioactive coatings, 3D-printed porous structures, and smart sensors that enhance osseointegration and monitor implant performance in real-time. Dental implants have advanced with the development of laser-structured surfaces, zirconia materials for improved biocompatibility, and guided implant surgery techniques that increase precision and reduce healing time. Both fields benefit from nanotechnology and customizable implant designs, driving improved patient outcomes and faster recovery periods.
Choosing the Right Implant: Factors for Patients and Surgeons
Choosing the right implant depends on anatomical location, load-bearing requirements, and biocompatibility, with orthopedic implants designed for large bone support and dental implants tailored for jawbone integration. Patient-specific factors such as bone density, overall health, and risk of infection critically influence implant selection and surgical planning. Surgeons prioritize implant materials like titanium or zirconia, ensuring optimal osseointegration and durability to maximize functional outcomes and reduce complication rates.
Orthopedic implant vs Dental implant Infographic
 productdif.com
productdif.com