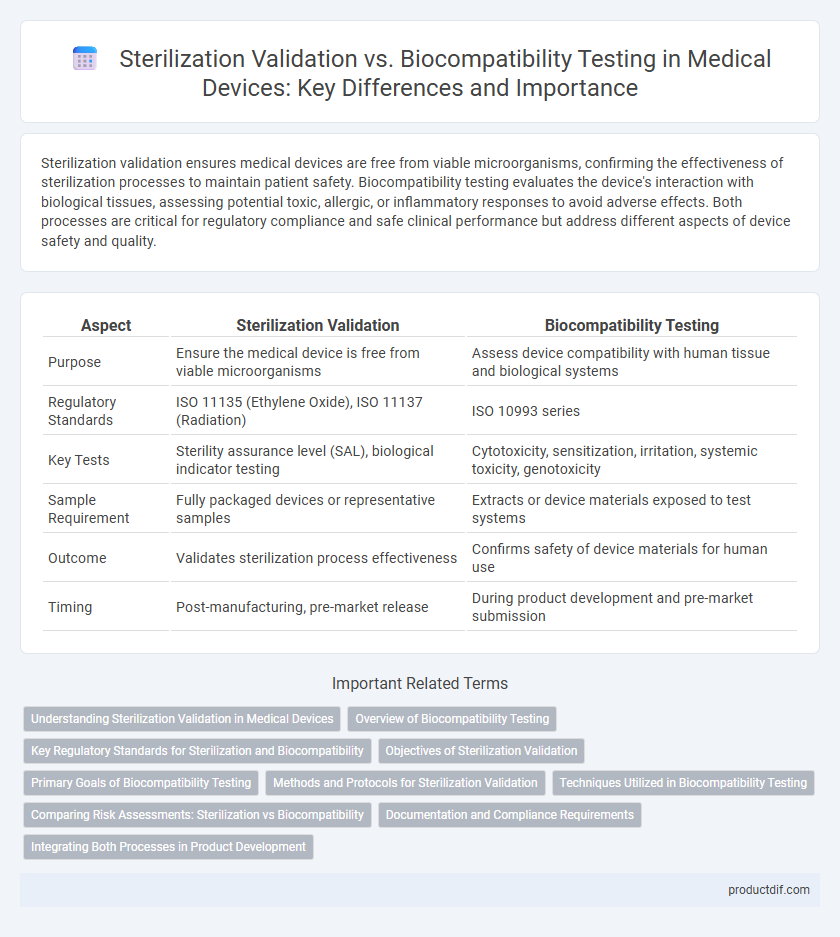
Sterilization validation ensures medical devices are free from viable microorganisms, confirming the effectiveness of sterilization processes to maintain patient safety. Biocompatibility testing evaluates the device's interaction with biological tissues, assessing potential toxic, allergic, or inflammatory responses to avoid adverse effects. Both processes are critical for regulatory compliance and safe clinical performance but address different aspects of device safety and quality.
Table of Comparison
| Aspect | Sterilization Validation | Biocompatibility Testing |
|---|---|---|
| Purpose | Ensure the medical device is free from viable microorganisms | Assess device compatibility with human tissue and biological systems |
| Regulatory Standards | ISO 11135 (Ethylene Oxide), ISO 11137 (Radiation) | ISO 10993 series |
| Key Tests | Sterility assurance level (SAL), biological indicator testing | Cytotoxicity, sensitization, irritation, systemic toxicity, genotoxicity |
| Sample Requirement | Fully packaged devices or representative samples | Extracts or device materials exposed to test systems |
| Outcome | Validates sterilization process effectiveness | Confirms safety of device materials for human use |
| Timing | Post-manufacturing, pre-market release | During product development and pre-market submission |
Understanding Sterilization Validation in Medical Devices
Sterilization validation in medical devices ensures the complete elimination of microbial contamination, verifying that sterilization processes meet regulatory standards such as ISO 11135 and ISO 17665. This validation involves establishing reproducible sterilization cycles through microbial indicators and bioburden assessments to guarantee device safety. Biocompatibility testing, by contrast, assesses the device material's interaction with biological tissues, focusing on cytotoxicity, sensitization, and irritation per ISO 10993 standards.
Overview of Biocompatibility Testing
Biocompatibility testing evaluates the interaction between a medical device and biological systems to ensure safety and compatibility with human tissues. It typically includes cytotoxicity, sensitization, irritation, and system toxicity assessments following ISO 10993 standards. This testing is critical for identifying potential adverse effects before clinical use, differentiating it from sterilization validation which focuses on microbial elimination.
Key Regulatory Standards for Sterilization and Biocompatibility
Sterilization validation adheres primarily to ISO 11135, ISO 11137, and ISO 17665 standards, ensuring complete microbial inactivation of medical devices. Biocompatibility testing follows ISO 10993 guidelines, evaluating biological responses to device materials to confirm safety for human use. Regulatory bodies such as the FDA and EMA require strict compliance with these standards to guarantee device efficacy and patient safety before market approval.
Objectives of Sterilization Validation
Sterilization validation aims to confirm that a medical device undergoes a reliable and effective sterilization process, eliminating all viable microorganisms to ensure patient safety. It involves establishing predefined sterilization parameters such as time, temperature, and sterilant concentration to achieve a sterility assurance level (SAL) of 10^-6. This validation ensures regulatory compliance and consistent product quality throughout the manufacturing lifecycle.
Primary Goals of Biocompatibility Testing
Biocompatibility testing primarily aims to evaluate the medical device's compatibility with human tissues and biological systems to prevent adverse reactions. This testing assesses cytotoxicity, sensitization, irritation, and systemic toxicity to ensure patient safety during device implantation or contact. Unlike sterilization validation that focuses on eliminating microorganisms, biocompatibility testing validates the material's safety profile in clinical use.
Methods and Protocols for Sterilization Validation
Sterilization validation involves rigorously testing methods such as biological indicators, chemical indicators, and physical parameter monitoring to ensure medical devices are free from viable microorganisms. Protocols typically include establishing sterilization cycles, conducting microbial load assessments, and performing validation runs under worst-case conditions to confirm efficacy and reproducibility. These methods are critical for compliance with regulatory standards like ISO 11135 and ISO 17665, which specify requirements for ethylene oxide and steam sterilization processes, respectively.
Techniques Utilized in Biocompatibility Testing
Biocompatibility testing utilizes techniques such as cytotoxicity assays, sensitization tests, and irritation evaluations to assess a medical device's compatibility with human tissues. Methods like ISO 10993 standards guide the use of in vitro and in vivo tests to detect potential adverse biological responses. These techniques ensure that materials do not induce toxicity, allergic reactions, or inflammation, which is distinct from sterilization validation that focuses on eliminating microbial contaminants.
Comparing Risk Assessments: Sterilization vs Biocompatibility
Sterilization validation risk assessments focus on ensuring microbial inactivation without compromising device functionality, targeting potential contamination hazards during manufacturing and use. Biocompatibility testing risk assessments evaluate toxicological and immunological responses to device materials, emphasizing patient safety through ISO 10993 standards. Comparing these assessments highlights sterilization's emphasis on microbial risk control versus biocompatibility's focus on material-host interactions, both critical for regulatory compliance and overall medical device safety.
Documentation and Compliance Requirements
Sterilization validation requires comprehensive documentation of sterilization cycles, biological indicators, and process parameters to demonstrate efficacy and regulatory compliance with standards such as ISO 11135 or ISO 17665. Biocompatibility testing documentation must include detailed reports of cytotoxicity, sensitization, and irritation assays in accordance with ISO 10993 to ensure material safety for patient contact. Both processes mandate strict adherence to FDA and ISO regulations, with traceable records for audit readiness and product approval.
Integrating Both Processes in Product Development
Integrating sterilization validation and biocompatibility testing in medical device development ensures comprehensive safety and performance evaluation. Sterilization validation confirms the effectiveness of microbial elimination methods, while biocompatibility testing assesses the device's interaction with human tissues and fluids. Coordinating these processes streamlines regulatory compliance and enhances product reliability by addressing potential material changes caused by sterilization methods early in the development cycle.
Sterilization validation vs Biocompatibility testing Infographic
 productdif.com
productdif.com