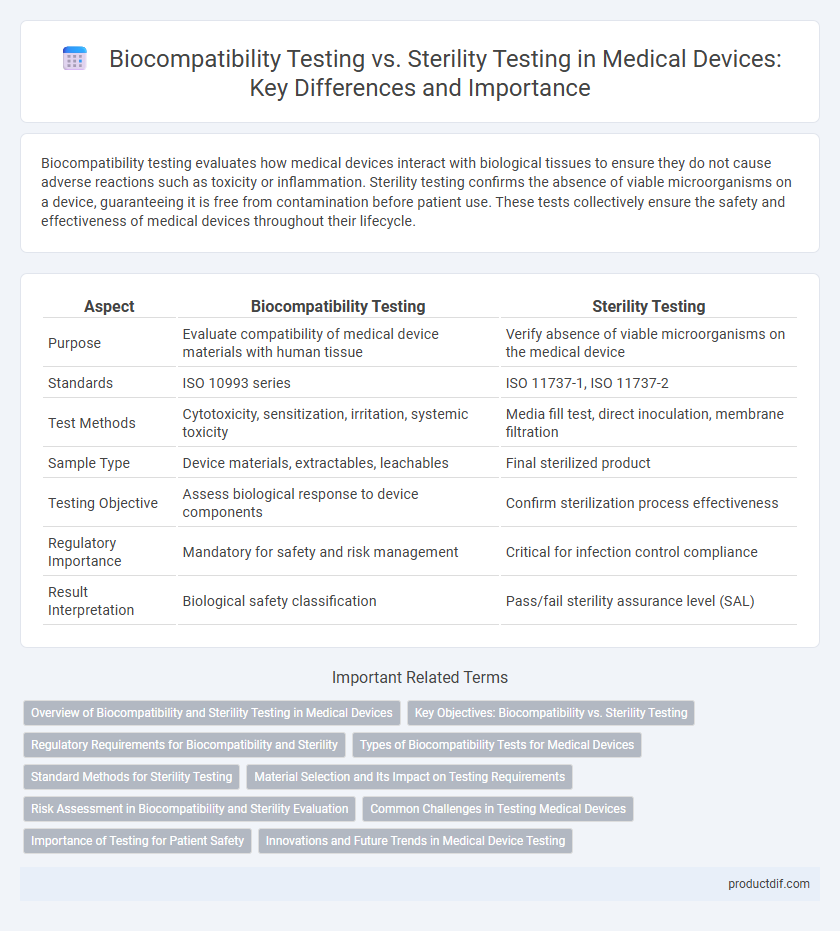
Biocompatibility testing evaluates how medical devices interact with biological tissues to ensure they do not cause adverse reactions such as toxicity or inflammation. Sterility testing confirms the absence of viable microorganisms on a device, guaranteeing it is free from contamination before patient use. These tests collectively ensure the safety and effectiveness of medical devices throughout their lifecycle.
Table of Comparison
| Aspect | Biocompatibility Testing | Sterility Testing |
|---|---|---|
| Purpose | Evaluate compatibility of medical device materials with human tissue | Verify absence of viable microorganisms on the medical device |
| Standards | ISO 10993 series | ISO 11737-1, ISO 11737-2 |
| Test Methods | Cytotoxicity, sensitization, irritation, systemic toxicity | Media fill test, direct inoculation, membrane filtration |
| Sample Type | Device materials, extractables, leachables | Final sterilized product |
| Testing Objective | Assess biological response to device components | Confirm sterilization process effectiveness |
| Regulatory Importance | Mandatory for safety and risk management | Critical for infection control compliance |
| Result Interpretation | Biological safety classification | Pass/fail sterility assurance level (SAL) |
Overview of Biocompatibility and Sterility Testing in Medical Devices
Biocompatibility testing evaluates the interaction between medical devices and biological tissues to ensure safety and minimize adverse reactions, focusing on cytotoxicity, sensitization, and irritation potential. Sterility testing verifies the absence of viable microorganisms on or within medical devices, utilizing methods such as membrane filtration and direct inoculation to confirm aseptic conditions. Both testing types are critical for regulatory compliance under ISO 10993 and ISO 11737 standards, ensuring devices are safe and sterile for patient use.
Key Objectives: Biocompatibility vs. Sterility Testing
Biocompatibility testing evaluates the interaction between medical devices and biological systems to ensure materials do not induce toxic, allergic, or inflammatory responses, prioritizing patient safety and regulatory compliance. Sterility testing focuses on verifying the absence of viable microorganisms on medical devices to prevent infections during use, meeting stringent healthcare standards. Both testing types are critical for device approval but address distinct safety dimensions: biological compatibility versus microbial contamination control.
Regulatory Requirements for Biocompatibility and Sterility
Regulatory requirements for biocompatibility testing mandate evaluation of a medical device's interaction with biological systems to ensure safety, guided primarily by ISO 10993 standards and FDA guidelines. Sterility testing regulations require validation of aseptic processing or terminal sterilization methods according to standards such as USP <71> and ISO 11737 to confirm absence of viable microorganisms. Compliance with these regulations is critical for obtaining market approval and maintaining patient safety in medical device manufacturing.
Types of Biocompatibility Tests for Medical Devices
Biocompatibility testing for medical devices includes cytotoxicity, sensitization, irritation, systemic toxicity, genotoxicity, and implantation tests to ensure materials do not produce harmful biological responses. Sterility testing, on the other hand, verifies the absence of viable microorganisms on or in the device, typically using methods like direct inoculation or membrane filtration. These biocompatibility tests are essential to evaluate the safety of materials in contact with body tissues, while sterility tests confirm the device's microbial safety before clinical use.
Standard Methods for Sterility Testing
Standard methods for sterility testing in medical devices, governed by ISO 11737 and USP <71>, focus on verifying the absence of viable microorganisms to ensure patient safety. Biocompatibility testing assesses the device's interaction with biological systems, whereas sterility testing strictly evaluates microbial contamination through methods like membrane filtration or direct inoculation. Adherence to validated protocols and environmental controls is critical to meet regulatory requirements and maintain device efficacy.
Material Selection and Its Impact on Testing Requirements
Material selection in medical devices critically influences biocompatibility and sterility testing requirements due to the varying chemical and physical properties of device materials. Biocompatibility testing assesses the potential toxic, allergic, or inflammatory responses elicited by device materials, necessitating thorough analysis when selecting polymers, metals, or ceramics. Sterility testing, on the other hand, is impacted by material porosity and surface characteristics that affect microbial contamination risk, dictating specific sterilization methods and validation protocols.
Risk Assessment in Biocompatibility and Sterility Evaluation
Risk assessment in biocompatibility testing evaluates the potential toxicological and immunological reactions of medical devices with human tissues to ensure patient safety, considering factors like material composition and exposure duration. In sterility testing, risk assessment focuses on identifying contamination sources and verifying the effectiveness of sterilization processes to prevent microbial presence in the final product. Integrating risk assessment results from both biocompatibility and sterility evaluations ensures comprehensive device safety and regulatory compliance throughout the medical device lifecycle.
Common Challenges in Testing Medical Devices
Biocompatibility testing and sterility testing both face common challenges such as ensuring accurate simulation of in vivo conditions and maintaining consistent testing environments. Cross-contamination risks and variability in biological responses complicate results, requiring stringent controls and validation methods. Regulatory compliance demands comprehensive documentation and reproducibility to prove safety and efficacy in medical device manufacturing.
Importance of Testing for Patient Safety
Biocompatibility testing ensures that medical devices do not provoke adverse biological responses when in contact with body tissues or fluids, reducing risks such as toxicity, irritation, or sensitization. Sterility testing verifies that devices are free from viable microorganisms, preventing infections and ensuring a sterile barrier during medical procedures. Together, these tests are critical for patient safety, helping to maintain device efficacy and minimize post-implantation complications.
Innovations and Future Trends in Medical Device Testing
Biocompatibility testing is evolving with innovations such as advanced in vitro models and computational toxicology to predict biological responses more accurately, while sterility testing is increasingly integrating rapid microbiological methods like PCR and real-time imaging for faster results. Emerging trends emphasize combining multi-omics technologies and artificial intelligence to optimize both biocompatibility and sterility assessments, enhancing safety profiles and regulatory compliance. Future advancements aim to develop non-destructive, automated testing platforms that reduce time and cost, accelerating the medical device development lifecycle.
Biocompatibility testing vs Sterility testing Infographic
 productdif.com
productdif.com