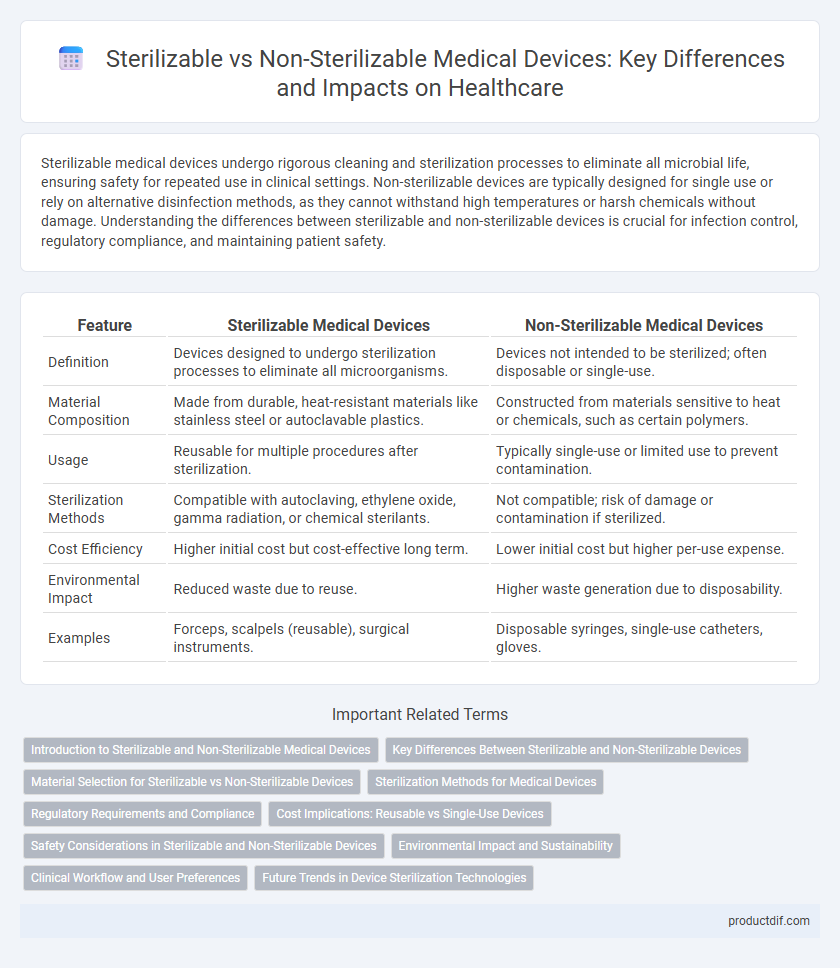
Sterilizable medical devices undergo rigorous cleaning and sterilization processes to eliminate all microbial life, ensuring safety for repeated use in clinical settings. Non-sterilizable devices are typically designed for single use or rely on alternative disinfection methods, as they cannot withstand high temperatures or harsh chemicals without damage. Understanding the differences between sterilizable and non-sterilizable devices is crucial for infection control, regulatory compliance, and maintaining patient safety.
Table of Comparison
| Feature | Sterilizable Medical Devices | Non-Sterilizable Medical Devices |
|---|---|---|
| Definition | Devices designed to undergo sterilization processes to eliminate all microorganisms. | Devices not intended to be sterilized; often disposable or single-use. |
| Material Composition | Made from durable, heat-resistant materials like stainless steel or autoclavable plastics. | Constructed from materials sensitive to heat or chemicals, such as certain polymers. |
| Usage | Reusable for multiple procedures after sterilization. | Typically single-use or limited use to prevent contamination. |
| Sterilization Methods | Compatible with autoclaving, ethylene oxide, gamma radiation, or chemical sterilants. | Not compatible; risk of damage or contamination if sterilized. |
| Cost Efficiency | Higher initial cost but cost-effective long term. | Lower initial cost but higher per-use expense. |
| Environmental Impact | Reduced waste due to reuse. | Higher waste generation due to disposability. |
| Examples | Forceps, scalpels (reusable), surgical instruments. | Disposable syringes, single-use catheters, gloves. |
Introduction to Sterilizable and Non-Sterilizable Medical Devices
Sterilizable medical devices are designed to withstand high-temperature steam, chemical, or radiation sterilization methods to ensure the elimination of all microorganisms, making them suitable for repeated use in sterile environments. Non-sterilizable medical devices, often intended for single use, cannot endure standard sterilization processes without damage, posing a greater risk of contamination if reused. Understanding the material composition and intended application of these devices is critical for effective infection control and patient safety in clinical settings.
Key Differences Between Sterilizable and Non-Sterilizable Devices
Sterilizable medical devices are designed to withstand high temperatures, chemicals, or radiation used during sterilization processes, ensuring they can be reused safely without compromising patient safety. Non-sterilizable devices are typically single-use or made from materials that degrade under sterilization conditions, increasing the risk of contamination if reused. The key differences lie in material composition, reprocessing capabilities, and regulatory requirements for maintaining sterility and preventing infection.
Material Selection for Sterilizable vs Non-Sterilizable Devices
Material selection for sterilizable medical devices prioritizes heat-resistant polymers like polyetheretherketone (PEEK) and metals such as stainless steel, which maintain structural integrity and biocompatibility after repeated sterilization cycles. Non-sterilizable devices often utilize cost-effective materials like low-density polyethylene (LDPE) or polypropylene (PP) that lack the thermal stability required for sterilization but are suitable for single-use applications. Understanding polymer thermal properties, such as glass transition temperature and chemical resistance, is critical in optimizing device longevity and safety in clinical settings.
Sterilization Methods for Medical Devices
Sterilization methods for medical devices include steam autoclaving, ethylene oxide (EO) gas, hydrogen peroxide plasma, and gamma radiation, each selected based on the device's material compatibility and sterilization requirements. Sterilizable devices must withstand high temperatures, moisture, or chemical exposure without degradation, while non-sterilizable devices are typically single-use or require alternative disinfection methods. Proper selection of sterilization ensures device safety, efficacy, and compliance with regulatory standards such as ISO 11135 for EO and ISO 17665 for steam sterilization.
Regulatory Requirements and Compliance
Sterilizable medical devices must comply with stringent regulatory requirements such as ISO 13485 and FDA 21 CFR Part 820, which mandate validated sterilization processes and detailed documentation to ensure patient safety. Non-sterilizable devices typically fall under different regulatory pathways, emphasizing biocompatibility and packaging integrity without the need for sterilization validation. Compliance for sterilizable devices also demands regular monitoring of sterilization efficacy, including biological indicators and cycle validation reports, to meet global standards and avoid product recalls.
Cost Implications: Reusable vs Single-Use Devices
Sterilizable medical devices often entail higher upfront costs due to durable materials and complex designs, but they offer long-term savings through multiple use cycles and reduced waste disposal expenses. Non-sterilizable single-use devices present lower initial investment but increase recurring costs related to frequent purchases, inventory management, and regulatory compliance for disposal. Cost implications must balance sterilization processes, infection control standards, and hospital budget constraints to optimize device selection.
Safety Considerations in Sterilizable and Non-Sterilizable Devices
Sterilizable medical devices undergo validated sterilization processes such as autoclaving or gamma irradiation, which effectively eliminate pathogens and reduce infection risks during patient use. Non-sterilizable devices often rely on single-use designs or disposable components to prevent contamination, requiring strict adherence to handling protocols to maintain safety. Choosing between sterilizable and non-sterilizable devices depends on factors like intended use, material biocompatibility, and regulatory compliance to ensure optimal patient safety.
Environmental Impact and Sustainability
Sterilizable medical devices typically contribute less to environmental waste compared to non-sterilizable, single-use products due to their reusability, reducing the demand for raw materials and minimizing landfill accumulation. The energy consumption and chemical use involved in sterilization processes must be optimized to enhance sustainability and lower the carbon footprint of reusable devices. Non-sterilizable devices, while convenient, generate higher volumes of medical waste requiring energy-intensive disposal methods such as incineration, leading to increased greenhouse gas emissions and resource depletion.
Clinical Workflow and User Preferences
Sterilizable medical devices enhance clinical workflow by enabling repeated use in sterile environments, reducing the need for frequent replacements and minimizing contamination risks. Non-sterilizable devices, often preferred for single-use scenarios, offer convenience and eliminate sterilization downtime but may increase waste and procurement costs. User preferences typically favor sterilizable tools in high-volume settings for cost-efficiency and sustainability, while non-sterilizable options suit emergency or low-frequency procedures requiring immediate availability.
Future Trends in Device Sterilization Technologies
Emerging sterilization technologies for medical devices emphasize low-temperature methods such as vaporized hydrogen peroxide and ozone plasma, enhancing compatibility with heat-sensitive materials. Advances in sterilizable device design integrate antimicrobial coatings and smart sensors to verify sterilization efficacy in real-time. Non-sterilizable device trends focus on single-use disposables with biodegradable materials to address infection control and environmental sustainability challenges.
Sterilizable vs Non-sterilizable Infographic
 productdif.com
productdif.com