Biocompatibility testing ensures that medical devices do not cause adverse biological reactions when in contact with the human body, assessing factors such as cytotoxicity, sensitization, and irritation. Shelf-life testing evaluates the stability, performance, and safety of the device over time under specified storage conditions to guarantee effectiveness until the expiration date. Both tests are critical for regulatory compliance and patient safety, but biocompatibility focuses on biological interactions while shelf-life testing centers on product durability and functionality.
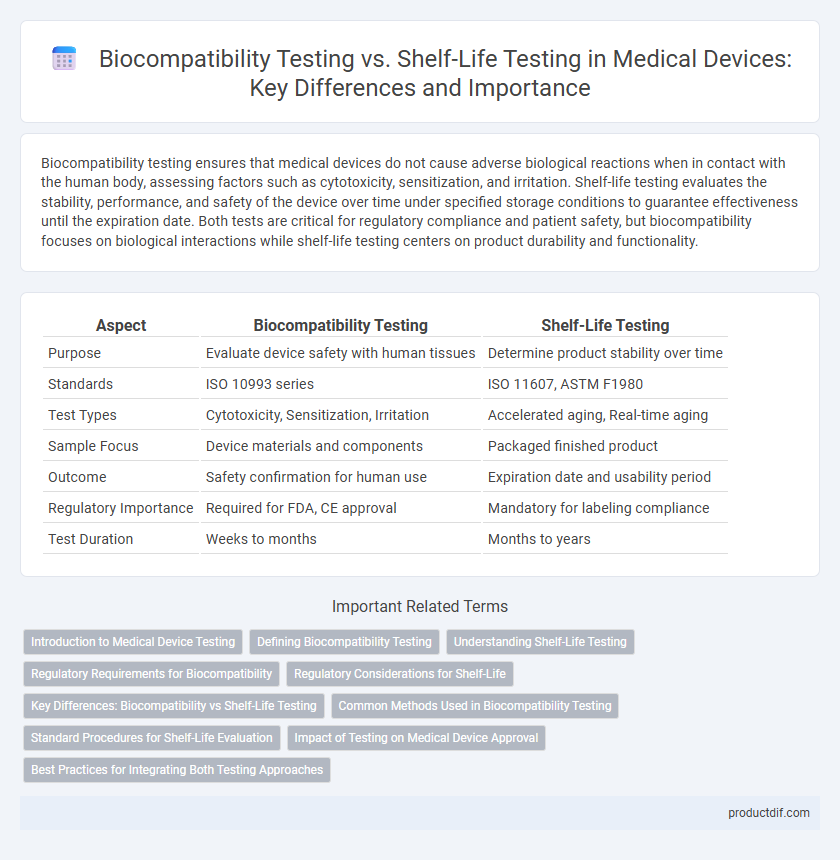
Table of Comparison
| Aspect | Biocompatibility Testing | Shelf-Life Testing |
|---|---|---|
| Purpose | Evaluate device safety with human tissues | Determine product stability over time |
| Standards | ISO 10993 series | ISO 11607, ASTM F1980 |
| Test Types | Cytotoxicity, Sensitization, Irritation | Accelerated aging, Real-time aging |
| Sample Focus | Device materials and components | Packaged finished product |
| Outcome | Safety confirmation for human use | Expiration date and usability period |
| Regulatory Importance | Required for FDA, CE approval | Mandatory for labeling compliance |
| Test Duration | Weeks to months | Months to years |
Introduction to Medical Device Testing
Medical device testing encompasses critical evaluations such as biocompatibility testing and shelf-life testing to ensure safety and effectiveness. Biocompatibility testing assesses the interaction between the device materials and biological tissues, identifying potential toxicity or adverse reactions. Shelf-life testing determines the duration a medical device maintains its functionality and sterility under specified storage conditions, guaranteeing reliability throughout its intended use period.
Defining Biocompatibility Testing
Biocompatibility testing evaluates how a medical device interacts with biological systems to ensure it does not provoke adverse reactions when implanted or in contact with body tissues. This testing assesses cytotoxicity, sensitization, irritation, and systemic toxicity based on ISO 10993 standards. Unlike shelf-life testing, which measures the device's stability and performance over time, biocompatibility testing focuses on patient safety through biological compatibility.
Understanding Shelf-Life Testing
Shelf-life testing determines the period a medical device maintains its safety, quality, and performance under specified storage conditions. This process involves accelerated aging studies, real-time stability assessments, and packaging integrity evaluations to ensure device reliability until the expiration date. Proper shelf-life validation is critical for regulatory compliance and patient safety, differentiating it from biocompatibility testing, which assesses device interaction with biological systems.
Regulatory Requirements for Biocompatibility
Regulatory requirements for biocompatibility testing in medical devices ensure that materials in contact with the body do not induce adverse biological responses, following standards such as ISO 10993. This testing is mandatory before device approval, focusing on cytotoxicity, sensitization, and irritation to demonstrate patient safety. Shelf-life testing, by contrast, primarily assesses product stability and functionality over time, with fewer direct regulatory mandates related to biological safety.
Regulatory Considerations for Shelf-Life
Shelf-life testing for medical devices must comply with regulatory frameworks such as FDA's 21 CFR Part 820 and ISO 13485, ensuring device performance and safety over the product's intended storage period. Regulatory authorities require validated protocols demonstrating that devices maintain biocompatibility, functionality, and sterility throughout their shelf life. Comprehensive documentation, including stability data and risk assessments, supports regulatory submissions to prove device integrity until expiration.
Key Differences: Biocompatibility vs Shelf-Life Testing
Biocompatibility testing evaluates a medical device's interactions with biological systems to ensure safety and minimize adverse reactions, focusing on cytotoxicity, sensitization, and irritation. Shelf-life testing determines the duration a device maintains its functional, physical, and chemical properties under specified storage conditions, ensuring efficacy and stability over time. Key differences lie in biocompatibility's emphasis on biological response and safety, while shelf-life testing prioritizes product integrity and performance throughout the device's usable period.
Common Methods Used in Biocompatibility Testing
Common methods used in biocompatibility testing for medical devices include cytotoxicity, sensitization, and irritation tests, which evaluate cellular response, allergic potential, and tissue compatibility respectively. In vitro assays, such as the MTT or Agar Diffusion tests, rapidly assess cell viability and proliferation, while in vivo tests involve animal models to observe systemic toxicity and local effects. These methods ensure devices meet ISO 10993 standards, critical for patient safety before proceeding to shelf-life testing that evaluates device stability over time.
Standard Procedures for Shelf-Life Evaluation
Shelf-life testing for medical devices follows ISO 11607 and ISO 13485 standards to ensure product integrity and sterility over time. These procedures include accelerated aging, real-time aging, and periodic inspection of packaging and materials to verify performance and safety. Biocompatibility testing, in contrast, assesses the biological response of tissues to the device under ISO 10993 standards, focusing on cytotoxicity, sensitization, and irritation without evaluating shelf stability.
Impact of Testing on Medical Device Approval
Biocompatibility testing assesses the safety of medical devices by evaluating their interaction with biological tissues, ensuring they do not cause adverse reactions, which is critical for regulatory approval. Shelf-life testing determines the duration a medical device maintains its functionality and sterility under specified storage conditions, directly impacting the device's marketability and compliance with standards. Both testing types provide essential data to regulatory bodies like the FDA and ISO, influencing the approval process and ensuring patient safety and product reliability.
Best Practices for Integrating Both Testing Approaches
Integrating biocompatibility testing with shelf-life testing in medical devices requires a harmonized approach that ensures material safety throughout the product's lifespan. Best practices emphasize conducting biocompatibility assessments early in development alongside accelerated aging studies to identify potential degradation effects on biocompatibility. Continuous monitoring and validation of both tests within quality management systems guarantee device performance and patient safety over time.
Biocompatibility Testing vs Shelf-Life Testing Infographic
 productdif.com
productdif.com