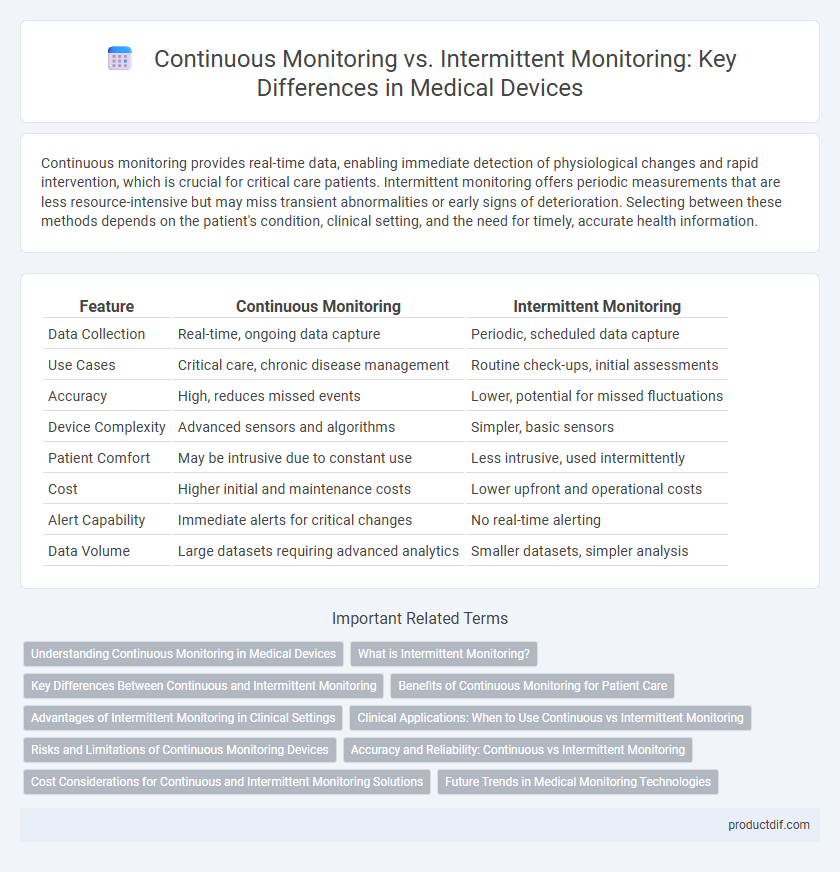
Continuous monitoring provides real-time data, enabling immediate detection of physiological changes and rapid intervention, which is crucial for critical care patients. Intermittent monitoring offers periodic measurements that are less resource-intensive but may miss transient abnormalities or early signs of deterioration. Selecting between these methods depends on the patient's condition, clinical setting, and the need for timely, accurate health information.
Table of Comparison
| Feature | Continuous Monitoring | Intermittent Monitoring |
|---|---|---|
| Data Collection | Real-time, ongoing data capture | Periodic, scheduled data capture |
| Use Cases | Critical care, chronic disease management | Routine check-ups, initial assessments |
| Accuracy | High, reduces missed events | Lower, potential for missed fluctuations |
| Device Complexity | Advanced sensors and algorithms | Simpler, basic sensors |
| Patient Comfort | May be intrusive due to constant use | Less intrusive, used intermittently |
| Cost | Higher initial and maintenance costs | Lower upfront and operational costs |
| Alert Capability | Immediate alerts for critical changes | No real-time alerting |
| Data Volume | Large datasets requiring advanced analytics | Smaller datasets, simpler analysis |
Understanding Continuous Monitoring in Medical Devices
Continuous monitoring in medical devices enables real-time tracking of vital signs such as heart rate, blood pressure, and oxygen saturation, providing comprehensive data for timely intervention. This approach leverages advanced sensors and wireless technology to deliver uninterrupted physiological data, improving patient outcomes in critical care and chronic disease management. Continuous monitoring supports proactive healthcare by detecting subtle changes and trends that intermittent monitoring might miss, enhancing diagnostic accuracy and therapeutic decisions.
What is Intermittent Monitoring?
Intermittent monitoring involves periodic assessment of a patient's vital signs or physiological parameters at specified intervals rather than continuously. This method typically uses devices such as manual blood pressure cuffs or handheld pulse oximeters, providing discrete data points that guide clinical decisions. Intermittent monitoring is preferred in settings where continuous data is not critical and allows for efficient resource utilization while maintaining patient safety.
Key Differences Between Continuous and Intermittent Monitoring
Continuous monitoring provides real-time data through sensors that track physiological parameters without interruption, allowing for immediate detection of critical changes in patient status. Intermittent monitoring relies on periodic checks at scheduled intervals, which may result in delayed response to acute events due to gaps in data collection. The key differences include data granularity, with continuous monitoring offering high-resolution insights, while intermittent monitoring prioritizes resource efficiency and simplicity in routine assessments.
Benefits of Continuous Monitoring for Patient Care
Continuous monitoring in medical devices enhances patient care by providing real-time, accurate data that enables early detection of critical changes in vital signs. This persistent data stream facilitates timely interventions, reducing the risk of complications and improving clinical outcomes. Continuous monitoring also supports personalized treatment plans by capturing comprehensive physiological trends compared to intermittent monitoring's snapshot approach.
Advantages of Intermittent Monitoring in Clinical Settings
Intermittent monitoring in clinical settings offers advantages such as reduced equipment costs and lower patient discomfort compared to continuous monitoring systems. It allows healthcare providers to perform targeted assessments during critical periods, optimizing resource allocation and minimizing unnecessary data overload. This approach is particularly beneficial in stable patients where continuous data is not essential, ensuring efficient clinical workflow and personalized patient care.
Clinical Applications: When to Use Continuous vs Intermittent Monitoring
Continuous monitoring provides real-time data critical for patients in intensive care units or those undergoing surgery, enabling immediate intervention for dynamic conditions like cardiac arrhythmias or respiratory distress. Intermittent monitoring suits stable patients in outpatient settings or routine check-ups, where periodic data collection suffices to assess chronic conditions such as hypertension or diabetes. Selecting between continuous and intermittent monitoring depends on clinical urgency, the severity of the condition, and resource availability to optimize patient outcomes.
Risks and Limitations of Continuous Monitoring Devices
Continuous monitoring devices in medical settings pose risks such as sensor inaccuracies, signal interference, and patient discomfort due to prolonged device attachment, potentially leading to false alarms or data loss. Battery dependency and technical malfunctions can result in monitoring gaps, compromising patient safety. Furthermore, continuous data streams require significant storage and processing capabilities, raising privacy and cybersecurity concerns.
Accuracy and Reliability: Continuous vs Intermittent Monitoring
Continuous monitoring devices provide real-time, accurate data by capturing physiological parameters without gaps, enhancing reliability in detecting rapid changes. Intermittent monitoring may miss critical events due to spaced measurements, reducing its accuracy and reliability for timely interventions. Advanced continuous monitoring systems utilize sensor technology and data analytics to ensure consistent and precise tracking of patient health metrics.
Cost Considerations for Continuous and Intermittent Monitoring Solutions
Continuous monitoring systems typically incur higher upfront costs due to advanced sensor technology and data integration capabilities, but they can reduce long-term expenses by enabling early detection of complications and minimizing hospital readmissions. Intermittent monitoring solutions, while generally less expensive initially, may lead to increased overall costs from delayed diagnosis and more frequent manual interventions. Evaluating total cost of ownership for each option requires considering device maintenance, data management, and patient outcome improvements associated with continuous versus intermittent monitoring in clinical settings.
Future Trends in Medical Monitoring Technologies
Continuous monitoring technologies are advancing rapidly with the integration of artificial intelligence and wearable sensors, enabling real-time data analysis and early detection of health anomalies. Intermittent monitoring remains relevant for cost-effective assessments but is increasingly complemented by continuous systems for comprehensive patient care. Future trends emphasize hybrid models combining continuous and intermittent data to improve diagnostic accuracy and personalized treatment plans.
Continuous monitoring vs Intermittent monitoring Infographic
 productdif.com
productdif.com