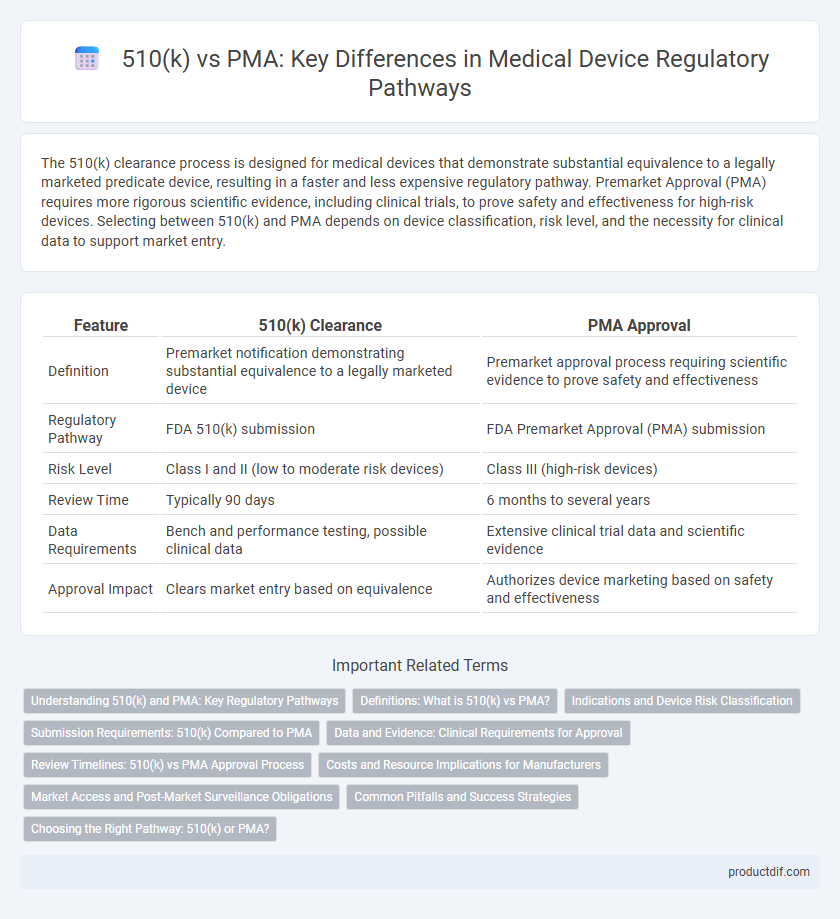
The 510(k) clearance process is designed for medical devices that demonstrate substantial equivalence to a legally marketed predicate device, resulting in a faster and less expensive regulatory pathway. Premarket Approval (PMA) requires more rigorous scientific evidence, including clinical trials, to prove safety and effectiveness for high-risk devices. Selecting between 510(k) and PMA depends on device classification, risk level, and the necessity for clinical data to support market entry.
Table of Comparison
| Feature | 510(k) Clearance | PMA Approval |
|---|---|---|
| Definition | Premarket notification demonstrating substantial equivalence to a legally marketed device | Premarket approval process requiring scientific evidence to prove safety and effectiveness |
| Regulatory Pathway | FDA 510(k) submission | FDA Premarket Approval (PMA) submission |
| Risk Level | Class I and II (low to moderate risk devices) | Class III (high-risk devices) |
| Review Time | Typically 90 days | 6 months to several years |
| Data Requirements | Bench and performance testing, possible clinical data | Extensive clinical trial data and scientific evidence |
| Approval Impact | Clears market entry based on equivalence | Authorizes device marketing based on safety and effectiveness |
Understanding 510(k) and PMA: Key Regulatory Pathways
510(k) and PMA are critical regulatory pathways established by the FDA for medical device approval, with 510(k) demonstrating substantial equivalence to a legally marketed device, commonly used for moderate-risk devices. PMA requires extensive clinical data proving safety and effectiveness, primarily for high-risk devices, demanding a more rigorous premarket approval process. Understanding the distinction between 510(k) and PMA ensures compliance with regulatory standards and facilitates efficient market entry for medical devices.
Definitions: What is 510(k) vs PMA?
510(k) is a premarket submission made to the FDA demonstrating that a medical device is substantially equivalent to a legally marketed device, allowing faster clearance for moderate-risk devices. Premarket Approval (PMA) is a rigorous FDA process that requires scientific evidence proving the safety and effectiveness of a high-risk medical device before it can be marketed. While 510(k) focuses on equivalence, PMA demands comprehensive clinical data and extensive review to ensure device safety.
Indications and Device Risk Classification
The 510(k) clearance pathway is designed for moderate-risk medical devices (Class II) with indications for use substantially equivalent to a legally marketed predicate device, ensuring safety and effectiveness through comparative data. In contrast, the Premarket Approval (PMA) process targets high-risk devices (Class III) with novel or critical indications, requiring comprehensive clinical trials and scientific evidence to demonstrate safety and efficacy. Device risk classification by the FDA directly influences the regulatory pathway, with Class II devices typically undergoing 510(k) review and Class III devices necessitating PMA submission due to their potential impact on patient health.
Submission Requirements: 510(k) Compared to PMA
The 510(k) submission requires demonstrating substantial equivalence to a legally marketed device, primarily focusing on safety and effectiveness through comparative data, and typically involves less extensive clinical evidence. The PMA (Pre-Market Approval) submission demands comprehensive scientific evidence, including rigorous clinical trials, detailed device descriptions, manufacturing processes, and safety evaluations to prove device effectiveness and safety. While 510(k) submissions generally involve shorter review timelines, PMA processes require more robust data and FDA scrutiny due to the higher risk class of devices involved.
Data and Evidence: Clinical Requirements for Approval
510(k) submissions primarily rely on demonstrating substantial equivalence to an existing legally marketed device, requiring limited clinical data or bench testing to support safety and effectiveness. In contrast, Premarket Approval (PMA) demands extensive clinical trial data, including statistically significant evidence of safety and efficacy, often through prospective, randomized controlled studies. The rigorous clinical requirements for PMA provide a higher level of evidence necessary for high-risk medical devices, while 510(k) is suitable for moderate-risk devices with well-established predicates.
Review Timelines: 510(k) vs PMA Approval Process
The 510(k) review process typically takes about 90 days, making it a faster route for medical device clearance, while the PMA approval process can extend from 180 days to over a year due to its rigorous evaluation of safety and effectiveness. A 510(k) is generally used for moderate-risk devices demonstrating substantial equivalence to a legally marketed device, whereas PMA is required for high-risk devices needing extensive clinical data. These differing timelines reflect the regulatory focus on device risk profiles and the level of evidence required for market authorization by the FDA.
Costs and Resource Implications for Manufacturers
510(k) submissions generally incur lower costs and require fewer resources compared to PMA (Premarket Approval), making them more accessible for manufacturers targeting moderate-risk medical devices. PMA involves extensive clinical trials, comprehensive documentation, and longer review times, leading to significantly higher expenses and greater resource allocation. Manufacturers must weigh the financial and operational impacts when selecting between 510(k) clearance and PMA approval pathways.
Market Access and Post-Market Surveillance Obligations
510(k) clearance allows for faster market access by demonstrating substantial equivalence to a predicate device, typically suited for moderate-risk medical devices. In contrast, PMA requires extensive clinical data and FDA review, leading to longer timeframes but is mandatory for high-risk devices. Post-market surveillance for PMA devices includes rigorous reporting and proactive studies, whereas 510(k) devices usually follow standard reporting obligations with fewer post-market requirements.
Common Pitfalls and Success Strategies
Navigating FDA approval pathways for medical devices requires understanding 510(k) and PMA differences, where common pitfalls include inadequate predicate device comparison in 510(k) and insufficient clinical data in PMA submissions. Success strategies emphasize thorough pre-submission meetings, robust clinical evidence generation, and comprehensive documentation aligning with FDA guidance. Leveraging regulatory expertise to address device-specific risks enhances approval efficiency and market entry speed.
Choosing the Right Pathway: 510(k) or PMA?
Choosing the right regulatory pathway between 510(k) and PMA depends on the risk classification and novelty of the medical device. The 510(k) process, suitable for moderate-risk devices substantially equivalent to existing products, offers faster clearance by demonstrating safety and effectiveness through comparative data. In contrast, the PMA pathway requires extensive clinical trials and rigorous evidence for high-risk, novel devices, ensuring a thorough assessment of safety and efficacy before market approval.
510(k) vs PMA Infographic
 productdif.com
productdif.com