Single-use devices offer the advantage of reducing the risk of cross-contamination and eliminating the need for sterilization, making them ideal for maintaining strict hygiene standards. In contrast, reusable devices require thorough cleaning and sterilization processes to ensure safety, which can increase operational costs but reduce environmental impact over time. Choosing between single-use and reusable equipment depends on factors such as infection control protocols, budget constraints, and sustainability goals.
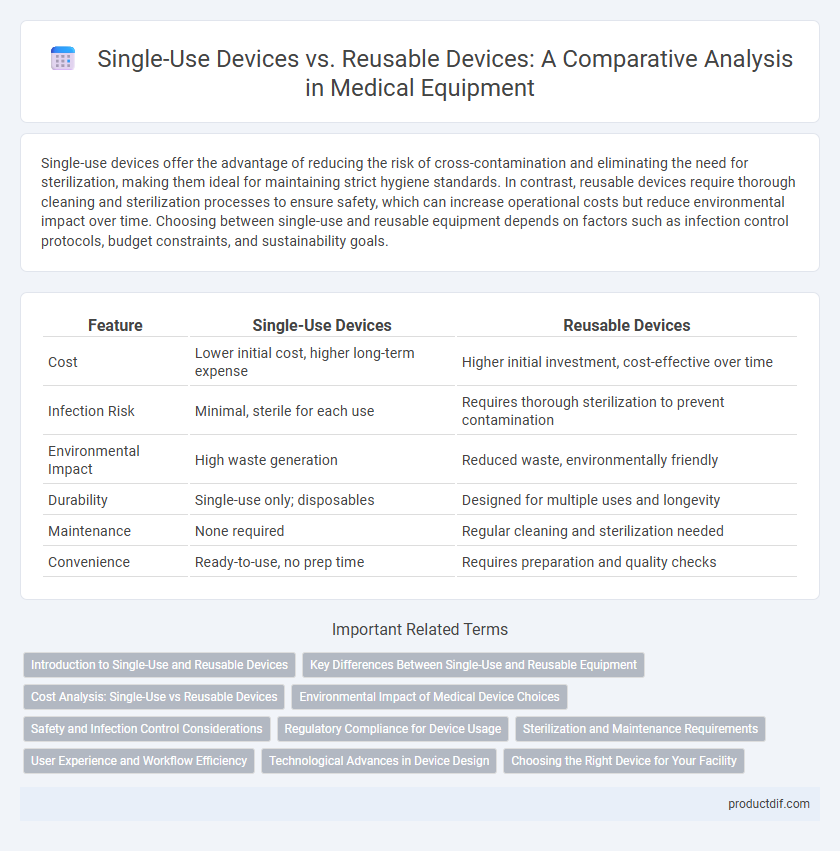
Table of Comparison
| Feature | Single-Use Devices | Reusable Devices |
|---|---|---|
| Cost | Lower initial cost, higher long-term expense | Higher initial investment, cost-effective over time |
| Infection Risk | Minimal, sterile for each use | Requires thorough sterilization to prevent contamination |
| Environmental Impact | High waste generation | Reduced waste, environmentally friendly |
| Durability | Single-use only; disposables | Designed for multiple uses and longevity |
| Maintenance | None required | Regular cleaning and sterilization needed |
| Convenience | Ready-to-use, no prep time | Requires preparation and quality checks |
Introduction to Single-Use and Reusable Devices
Single-use devices are designed for one-time application, minimizing infection risks and ensuring sterility, making them ideal for procedures demanding high hygiene standards. Reusable devices undergo sterilization after each use, offering cost-efficiency and environmental benefits but require stringent maintenance protocols to prevent contamination. Understanding the material composition and intended usage of each device type is crucial for selecting appropriate equipment in clinical and industrial settings.
Key Differences Between Single-Use and Reusable Equipment
Single-use devices are designed for one-time use to prevent cross-contamination and ensure sterility, making them ideal for infection control in medical settings. Reusable devices require thorough cleaning and sterilization after each use, offering cost-efficiency and sustainability but demanding strict maintenance protocols. Material durability and regulatory compliance are critical factors distinguishing these equipment types in healthcare and laboratory applications.
Cost Analysis: Single-Use vs Reusable Devices
Single-use devices typically incur higher long-term costs due to continuous replacement needs, while reusable devices require substantial initial investments but offer cost savings over time through multiple uses. Maintenance, sterilization, and training expenses significantly impact the overall cost-effectiveness of reusable devices. A comprehensive cost analysis must consider procurement, operational, and disposal costs to determine the most economically viable option for healthcare facilities.
Environmental Impact of Medical Device Choices
Single-use medical devices generate significant plastic waste and contribute to landfill accumulation, increasing environmental pollution and carbon footprint. Reusable devices reduce waste by allowing multiple sterilizations and extended lifespans, but require energy and water consumption for proper cleaning and maintenance. Evaluating the lifecycle environmental impact, including resource extraction, manufacturing, use, and disposal, is essential for sustainable medical device choices.
Safety and Infection Control Considerations
Single-use devices minimize the risk of cross-contamination by eliminating the need for sterilization, making them safer in infection control settings. Reusable devices require rigorous cleaning, disinfection, and sterilization protocols to prevent pathogen transmission, increasing the risk of human error. Healthcare facilities must balance cost-effectiveness with strict adherence to safety standards to reduce healthcare-associated infections (HAIs).
Regulatory Compliance for Device Usage
Regulatory compliance for single-use devices mandates strict adherence to labeling, disposal protocols, and prohibition of reuse to prevent contamination and infection risks. Reusable devices require rigorous validation of cleaning, sterilization processes, and maintenance documentation to meet standards set by agencies such as the FDA and ISO. Failure to comply with these regulatory requirements can result in significant legal penalties and compromise patient safety.
Sterilization and Maintenance Requirements
Single-use devices eliminate the need for sterilization and reduce the risk of cross-contamination, ensuring consistent safety but increasing medical waste. Reusable devices require rigorous sterilization protocols, including autoclaving or chemical disinfection, to maintain hygiene and functionality. Regular maintenance and inspection are critical for reusable equipment to prevent device degradation and ensure patient safety.
User Experience and Workflow Efficiency
Single-use devices offer streamlined workflows by eliminating the need for cleaning and sterilization, which enhances user experience through reduced preparation time and minimized infection risk. Reusable devices, while more cost-effective over time, require meticulous maintenance protocols that can interrupt clinical operations and increase the workload on staff. Balancing these factors, healthcare facilities must evaluate user preferences and procedural demands to optimize workflow efficiency and device reliability.
Technological Advances in Device Design
Technological advances in device design have significantly improved both single-use and reusable medical devices by integrating materials that enhance durability and sterility. Innovations such as antimicrobial coatings and modular components increase the safety and functionality of single-use devices while enabling easier sterilization and extended lifecycle for reusable equipment. Smart sensor technology embedded in these devices provides real-time monitoring and ensures optimal performance, reducing infection risks and operational costs.
Choosing the Right Device for Your Facility
Choosing between single-use devices and reusable devices depends on factors such as infection control protocols, cost-efficiency, and operational workflow. Single-use devices minimize cross-contamination risks and reduce sterilization time, making them ideal for high-risk environments or facilities with limited sterilization capabilities. Reusable devices offer long-term cost savings and environmental benefits but require stringent maintenance and sterilization processes to ensure patient safety.
Single-use devices vs reusable devices Infographic
 productdif.com
productdif.com