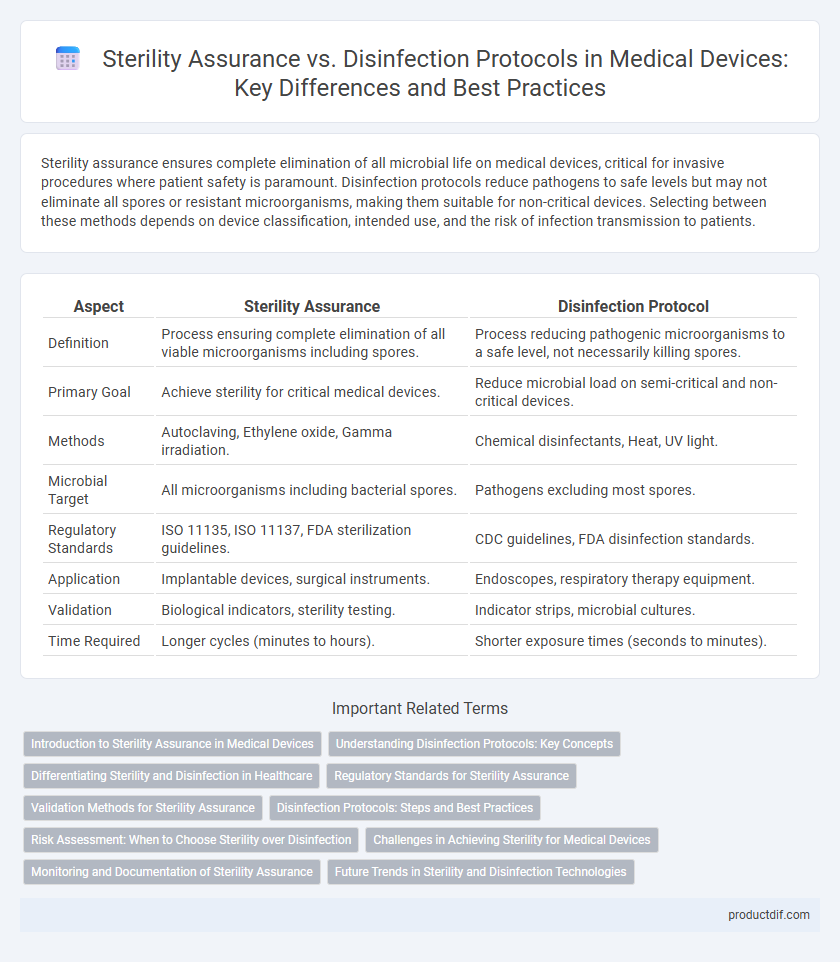
Sterility assurance ensures complete elimination of all microbial life on medical devices, critical for invasive procedures where patient safety is paramount. Disinfection protocols reduce pathogens to safe levels but may not eliminate all spores or resistant microorganisms, making them suitable for non-critical devices. Selecting between these methods depends on device classification, intended use, and the risk of infection transmission to patients.
Table of Comparison
| Aspect | Sterility Assurance | Disinfection Protocol |
|---|---|---|
| Definition | Process ensuring complete elimination of all viable microorganisms including spores. | Process reducing pathogenic microorganisms to a safe level, not necessarily killing spores. |
| Primary Goal | Achieve sterility for critical medical devices. | Reduce microbial load on semi-critical and non-critical devices. |
| Methods | Autoclaving, Ethylene oxide, Gamma irradiation. | Chemical disinfectants, Heat, UV light. |
| Microbial Target | All microorganisms including bacterial spores. | Pathogens excluding most spores. |
| Regulatory Standards | ISO 11135, ISO 11137, FDA sterilization guidelines. | CDC guidelines, FDA disinfection standards. |
| Application | Implantable devices, surgical instruments. | Endoscopes, respiratory therapy equipment. |
| Validation | Biological indicators, sterility testing. | Indicator strips, microbial cultures. |
| Time Required | Longer cycles (minutes to hours). | Shorter exposure times (seconds to minutes). |
Introduction to Sterility Assurance in Medical Devices
Sterility assurance in medical devices involves rigorous validation processes to ensure complete elimination of viable microorganisms, critical for patient safety and regulatory compliance. This includes monitoring sterilization parameters such as temperature, time, and microbial load to achieve a sterility assurance level (SAL) typically set at 10^-6. Disinfection protocols, while reducing microbial contamination, do not guarantee the sterility levels required for invasive medical devices, emphasizing the need for validated sterilization methods in manufacturing and healthcare settings.
Understanding Disinfection Protocols: Key Concepts
Disinfection protocols in medical device management focus on eliminating or reducing pathogenic microorganisms to safe levels without requiring sterilization. These protocols involve selecting appropriate disinfectants based on factors like activity spectrum, contact time, and device material compatibility. Understanding key parameters ensures effective microbial control while preserving device integrity and patient safety.
Differentiating Sterility and Disinfection in Healthcare
Sterility assurance ensures the complete elimination of all microorganisms, including spores, on medical devices using validated methods such as steam sterilization or ethylene oxide gas. Disinfection protocols reduce the number of pathogenic microorganisms to a safe level but do not guarantee the complete destruction of all microbial life, often relying on chemical agents like alcohol or chlorine-based solutions. Differentiating sterility from disinfection in healthcare settings is critical for preventing infections and selecting appropriate reprocessing procedures based on device classification and intended use.
Regulatory Standards for Sterility Assurance
Regulatory standards for sterility assurance in medical devices, such as ISO 11135 for ethylene oxide sterilization and ISO 11137 for radiation sterilization, establish strict criteria to ensure microbial inactivation and patient safety. Compliance with FDA guidelines and ANSI/AAMI ST79 consolidates best practices for process validation, including bioburden control and sterility testing, which are more rigorous than typical disinfection protocols. These standards require comprehensive documentation and routine monitoring to maintain validated sterile conditions, surpassing the requirements set for disinfection procedures that primarily reduce microbial load but do not guarantee sterility.
Validation Methods for Sterility Assurance
Validation methods for sterility assurance in medical devices involve rigorous biological indicator testing, including the use of standardized bacterial spores such as Geobacillus stearothermophilus to confirm sterilizer efficacy. Physical and chemical indicators complement biological tests by monitoring critical process parameters like temperature, time, and chemical concentration throughout sterilization cycles. These validation protocols are essential for ensuring compliance with ISO 11135 and ISO 11137 standards, providing quantifiable evidence that sterilization processes achieve the required sterility assurance level (SAL) of 10^-6.
Disinfection Protocols: Steps and Best Practices
Disinfection protocols in medical device management involve systematic steps including pre-cleaning, selection of appropriate disinfectants, application, contact time adherence, and thorough rinsing to ensure microbial reduction without compromising device integrity. Best practices emphasize compatibility testing of disinfectants with device materials, validation of procedures through microbial load monitoring, and training of personnel to maintain consistent compliance. Effective implementation of these protocols minimizes infection risks and prolongs device functionality by preventing contamination during reuse.
Risk Assessment: When to Choose Sterility over Disinfection
Risk assessment in medical device processing determines when sterility assurance must be prioritized over disinfection protocols to minimize patient infection risks. Devices classified as critical, such as surgical instruments that penetrate sterile tissues or the vascular system, require sterility to ensure no viable microorganisms remain. Non-critical devices contacting intact skin typically undergo disinfection, but risk analysis considers device use, patient vulnerability, and procedure type to select appropriate microbial control measures.
Challenges in Achieving Sterility for Medical Devices
Achieving sterility for medical devices presents significant challenges due to varying device materials and complex designs that hinder effective sterilant penetration. Sterility assurance requires validation of sterilization methods to ensure complete microorganism eradication, whereas disinfection protocols primarily reduce microbial load without guaranteeing total sterility. Inconsistent microbial resistance and potential device damage further complicate validating sterilization processes, making rigorous quality control and adherence to standards like ISO 11135 and ISO 17665 critical.
Monitoring and Documentation of Sterility Assurance
Sterility assurance in medical devices involves rigorous monitoring through validated biological indicators and continuous environmental controls to ensure contamination-free conditions. Detailed documentation of sterilization cycles, equipment maintenance logs, and batch traceability provides a comprehensive record that supports regulatory compliance and patient safety. In contrast, disinfection protocols typically rely on less stringent monitoring and documentation, emphasizing surface cleanliness rather than absolute microbial elimination.
Future Trends in Sterility and Disinfection Technologies
Emerging sterilization technologies such as low-temperature hydrogen peroxide plasma and vaporized peracetic acid are reshaping sterility assurance by enabling faster, more effective microbial inactivation with reduced material compatibility issues. Advances in UV-C LED and ozone-based disinfection systems offer scalable, eco-friendly alternatives that improve surface decontamination protocols while minimizing chemical residues. Integration of AI-driven monitoring systems enhances real-time validation and process control, setting new standards for reliability in medical device sterility and disinfection compliance.
Sterility assurance vs Disinfection protocol Infographic
 productdif.com
productdif.com