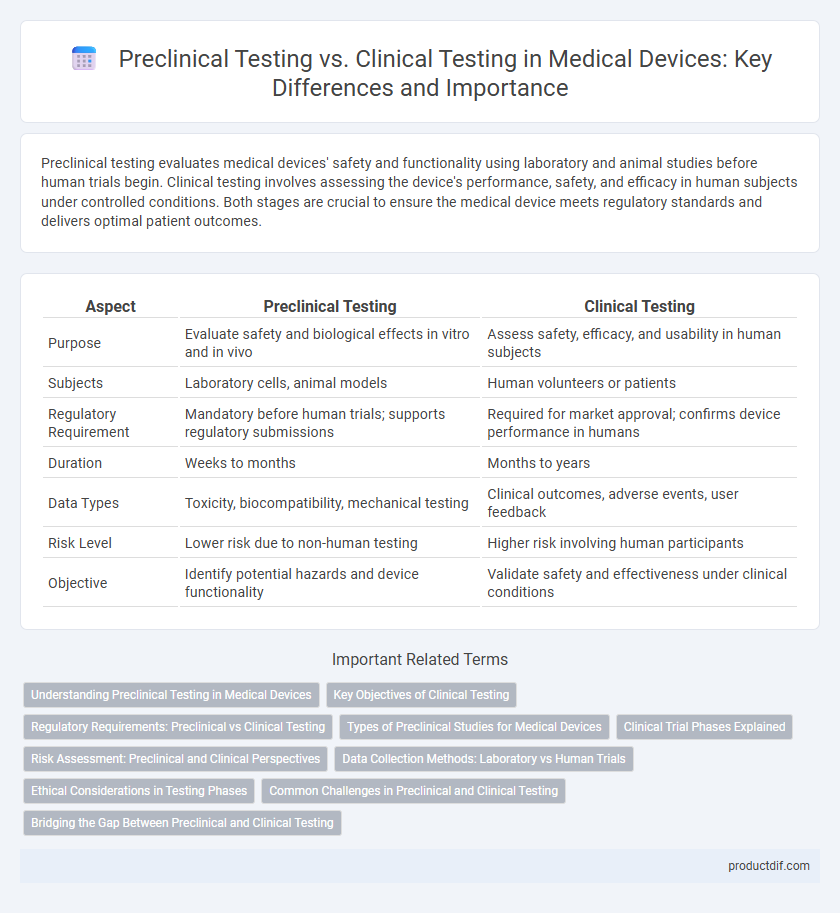
Preclinical testing evaluates medical devices' safety and functionality using laboratory and animal studies before human trials begin. Clinical testing involves assessing the device's performance, safety, and efficacy in human subjects under controlled conditions. Both stages are crucial to ensure the medical device meets regulatory standards and delivers optimal patient outcomes.
Table of Comparison
| Aspect | Preclinical Testing | Clinical Testing |
|---|---|---|
| Purpose | Evaluate safety and biological effects in vitro and in vivo | Assess safety, efficacy, and usability in human subjects |
| Subjects | Laboratory cells, animal models | Human volunteers or patients |
| Regulatory Requirement | Mandatory before human trials; supports regulatory submissions | Required for market approval; confirms device performance in humans |
| Duration | Weeks to months | Months to years |
| Data Types | Toxicity, biocompatibility, mechanical testing | Clinical outcomes, adverse events, user feedback |
| Risk Level | Lower risk due to non-human testing | Higher risk involving human participants |
| Objective | Identify potential hazards and device functionality | Validate safety and effectiveness under clinical conditions |
Understanding Preclinical Testing in Medical Devices
Preclinical testing in medical devices involves rigorous laboratory and animal studies to assess safety, functionality, and biocompatibility before human trials. This stage identifies potential risks, device performance, and biological responses, ensuring compliance with regulatory standards such as ISO 10993. Comprehensive preclinical data supports the device's transition to clinical testing by minimizing adverse effects and optimizing design for human use.
Key Objectives of Clinical Testing
Clinical testing aims to evaluate the safety, efficacy, and performance of medical devices in human subjects under real-world conditions. It involves assessing device functionality, identifying adverse effects, and gathering data to support regulatory approval and market entry. Ensuring patient safety and demonstrating clinical benefits are primary objectives during this phase.
Regulatory Requirements: Preclinical vs Clinical Testing
Regulatory requirements for medical devices mandate rigorous preclinical testing to evaluate safety and biocompatibility before clinical trials commence, ensuring the device meets essential performance standards. Clinical testing is then required to demonstrate efficacy and monitor adverse events in human subjects under controlled conditions, aligning with FDA and international guidelines such as ISO 14155. Compliance with both preclinical and clinical regulatory frameworks facilitates market approval and ongoing post-market surveillance.
Types of Preclinical Studies for Medical Devices
Preclinical testing for medical devices typically involves biocompatibility assessment, bench testing, and animal studies to evaluate safety and performance before human trials. Biocompatibility studies conform to ISO 10993 standards to ensure the device does not induce adverse tissue reactions. Mechanical and functional bench tests simulate device use conditions, while in vivo animal models provide data on device behavior in biological environments, guiding design optimization and risk mitigation.
Clinical Trial Phases Explained
Clinical trial phases for medical devices consist of Phase I (safety assessment with a small group of healthy volunteers), Phase II (efficacy and optimal usage evaluation in a larger patient population), and Phase III (large-scale testing to confirm effectiveness and monitor adverse reactions). Preclinical testing provides essential data on biocompatibility, mechanical performance, and toxicity before trials involving human subjects begin. Regulatory bodies such as the FDA require comprehensive clinical data from these phases to ensure device safety and effectiveness prior to market approval.
Risk Assessment: Preclinical and Clinical Perspectives
Preclinical testing involves laboratory and animal studies to evaluate the safety and biological effects of a medical device, providing critical data for initial risk assessment before human exposure. Clinical testing assesses device performance and potential risks in human subjects under controlled conditions, focusing on adverse event monitoring and real-world application outcomes. Comprehensive risk assessment integrates both preclinical toxicology and biomechanics data with clinical safety and efficacy results to ensure regulatory compliance and patient safety.
Data Collection Methods: Laboratory vs Human Trials
Preclinical testing relies on laboratory-based data collection methods such as in vitro assays and animal studies to evaluate the safety and efficacy of medical devices before human exposure. Clinical testing gathers data through controlled human trials, providing direct evidence of device performance, safety, and patient outcomes under real-world conditions. The transition from preclinical to clinical testing ensures comprehensive validation through progressively human-relevant data sets.
Ethical Considerations in Testing Phases
Preclinical testing involves extensive laboratory and animal studies to ensure the safety and efficacy of medical devices before human exposure, emphasizing minimizing harm and adhering to strict animal welfare regulations. Clinical testing requires obtaining informed consent from human subjects, ensuring patient safety, and safeguarding privacy, with continuous monitoring for adverse effects under regulatory oversight. Ethical considerations in both phases prioritize transparency, risk-benefit analysis, and compliance with international guidelines such as the Declaration of Helsinki.
Common Challenges in Preclinical and Clinical Testing
Preclinical testing often faces challenges such as replicating human physiological conditions accurately and ensuring biocompatibility of medical devices, which impacts the predictability of safety and efficacy. Clinical testing encounters difficulties in patient recruitment, adherence to regulatory standards, and managing variability in human responses that can affect outcome reliability. Both testing phases struggle with data interpretation complexity and maintaining consistent quality control to support successful device approval and market entry.
Bridging the Gap Between Preclinical and Clinical Testing
Preclinical testing in medical devices involves in vitro and animal studies to evaluate safety, biocompatibility, and initial functionality before human trials, whereas clinical testing assesses the device's safety and effectiveness in human subjects under controlled conditions. Bridging the gap between preclinical and clinical testing requires robust translational strategies, including validated animal models that closely mimic human physiology and predictive biomarkers to anticipate clinical outcomes. Effective integration of preclinical data with clinical trial design ensures regulatory compliance, accelerates device approval, and enhances patient safety during first-in-human applications.
Preclinical Testing vs Clinical Testing Infographic
 productdif.com
productdif.com