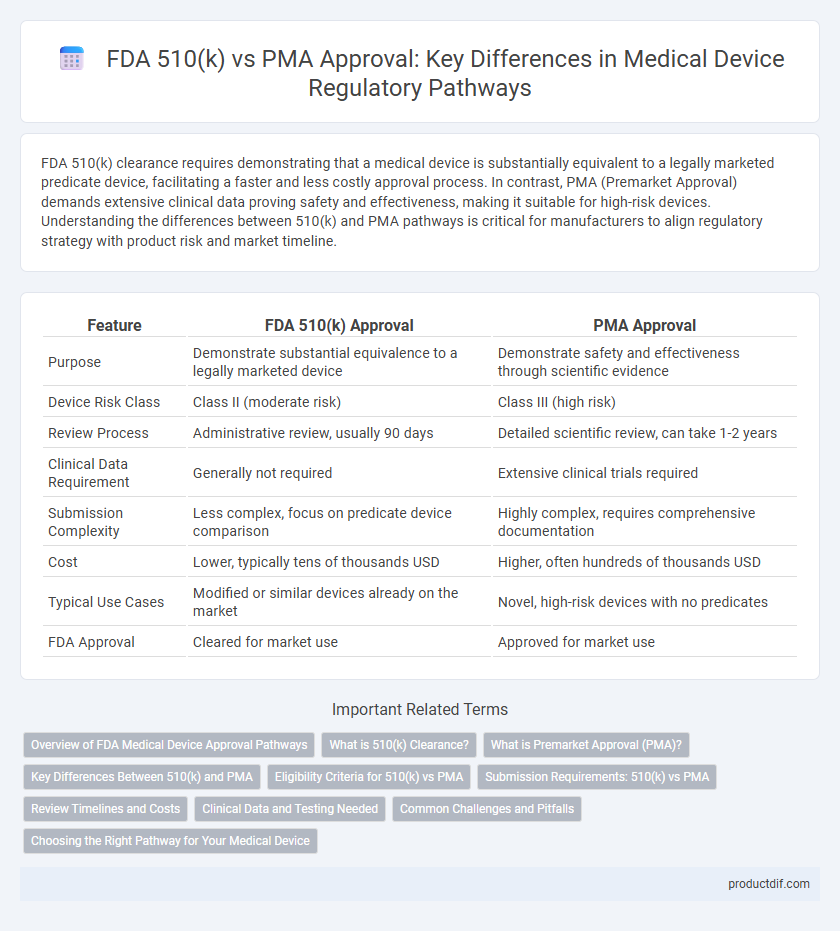
FDA 510(k) clearance requires demonstrating that a medical device is substantially equivalent to a legally marketed predicate device, facilitating a faster and less costly approval process. In contrast, PMA (Premarket Approval) demands extensive clinical data proving safety and effectiveness, making it suitable for high-risk devices. Understanding the differences between 510(k) and PMA pathways is critical for manufacturers to align regulatory strategy with product risk and market timeline.
Table of Comparison
| Feature | FDA 510(k) Approval | PMA Approval |
|---|---|---|
| Purpose | Demonstrate substantial equivalence to a legally marketed device | Demonstrate safety and effectiveness through scientific evidence |
| Device Risk Class | Class II (moderate risk) | Class III (high risk) |
| Review Process | Administrative review, usually 90 days | Detailed scientific review, can take 1-2 years |
| Clinical Data Requirement | Generally not required | Extensive clinical trials required |
| Submission Complexity | Less complex, focus on predicate device comparison | Highly complex, requires comprehensive documentation |
| Cost | Lower, typically tens of thousands USD | Higher, often hundreds of thousands USD |
| Typical Use Cases | Modified or similar devices already on the market | Novel, high-risk devices with no predicates |
| FDA Approval | Cleared for market use | Approved for market use |
Overview of FDA Medical Device Approval Pathways
The FDA medical device approval pathways include the 510(k) premarket notification and the Premarket Approval (PMA) processes, differing primarily in risk classification and evidence requirements. The 510(k) pathway applies to moderate-risk devices that demonstrate substantial equivalence to a legally marketed predicate, facilitating faster market entry. PMA is reserved for high-risk devices, necessitating rigorous clinical data to establish safety and effectiveness before FDA clearance.
What is 510(k) Clearance?
510(k) clearance is a premarket submission made to the FDA to demonstrate that a medical device is substantially equivalent to a legally marketed predicate device, allowing it to enter the market without extensive clinical trials required for Premarket Approval (PMA). This process is generally faster and less costly than PMA, primarily used for moderate-risk devices classified as Class II. FDA 510(k) clearance ensures the safety and effectiveness of devices based on comparison rather than new evidence of clinical benefits.
What is Premarket Approval (PMA)?
Premarket Approval (PMA) is the FDA's most stringent regulatory process for medical devices, required for Class III devices that support or sustain human life or present a potential risk of illness or injury. This approval mandates comprehensive scientific evidence, including clinical trial data, to demonstrate safety and effectiveness before marketing. PMA involves rigorous review of manufacturing processes, labeling, and post-market surveillance plans to ensure ongoing device performance and patient safety.
Key Differences Between 510(k) and PMA
The FDA 510(k) process requires demonstrating that a medical device is substantially equivalent to a legally marketed predicate device, typically resulting in faster clearance times averaging 90 days. Premarket Approval (PMA) involves a more rigorous scientific review, including clinical data to establish safety and effectiveness, with approval timelines often extending beyond one year. Key differences include the level of evidence required, complexity of submission, and regulatory scrutiny, where PMA targets high-risk (Class III) devices and 510(k) commonly applies to moderate-risk (Class II) devices.
Eligibility Criteria for 510(k) vs PMA
Eligibility criteria for FDA 510(k) clearance require that the medical device be substantially equivalent to a legally marketed predicate device, typically classified as Class II or some Class I devices with low to moderate risk. In contrast, PMA approval applies to Class III devices that support or sustain human life, present significant risk, or lack a predicate, necessitating more rigorous clinical data and scientific evidence. The 510(k) pathway favors devices with well-established technology, while PMA targets innovative or high-risk medical devices requiring comprehensive safety and effectiveness demonstration.
Submission Requirements: 510(k) vs PMA
FDA 510(k) submission requires demonstrating substantial equivalence to a legally marketed predicate device, typically including device description, intended use, performance testing, and labeling information. PMA submission demands comprehensive scientific evidence of safety and effectiveness, including clinical data, detailed device design, manufacturing processes, and risk analysis. The 510(k) process is generally faster and less burdensome, while the PMA involves rigorous, in-depth documentation and review.
Review Timelines and Costs
FDA 510(k) clearance typically involves a review timeline of 90 days, making it faster compared to Premarket Approval (PMA), which can take 180 days to over a year due to its rigorous evaluation process. Costs for 510(k) submissions are generally lower, often ranging from $5,000 to $15,000, whereas PMA applications can exceed $250,000 due to extensive clinical data requirements and thorough FDA scrutiny. These differences reflect the risk classification of medical devices, with 510(k) used for moderate-risk devices and PMA reserved for high-risk Class III devices.
Clinical Data and Testing Needed
FDA 510(k) clearance primarily requires demonstrating substantial equivalence to a legally marketed device, often relying on bench testing and limited clinical data, whereas PMA approval demands comprehensive clinical trials providing rigorous safety and effectiveness evidence. The PMA process involves extensive preclinical studies, detailed manufacturing information, and often multiple phases of human clinical testing to meet stringent FDA standards. Devices with higher risk profiles typically undergo PMA review due to the necessity for in-depth clinical data and validation.
Common Challenges and Pitfalls
Navigating FDA 510(k) and PMA approval processes poses common challenges such as differing evidentiary requirements, with 510(k) focusing on substantial equivalence and PMA demanding extensive clinical data. Misinterpretation of submission criteria often leads to delays or rejection, highlighting the need for thorough documentation and risk analysis. Understanding the varying timelines and costs associated with both pathways is critical to avoiding pitfalls in medical device market entry.
Choosing the Right Pathway for Your Medical Device
Selecting the appropriate FDA approval pathway, either 510(k) or PMA, depends on the device's risk classification and intended use, with 510(k) primarily for moderate-risk devices demonstrating substantial equivalence to a legally marketed device. Premarket Approval (PMA) is required for high-risk Class III devices, demanding robust clinical evidence to ensure safety and effectiveness. Understanding device classification and regulatory requirements accelerates market entry and compliance for medical device manufacturers.
FDA 510(k) vs PMA Approval Infographic
 productdif.com
productdif.com