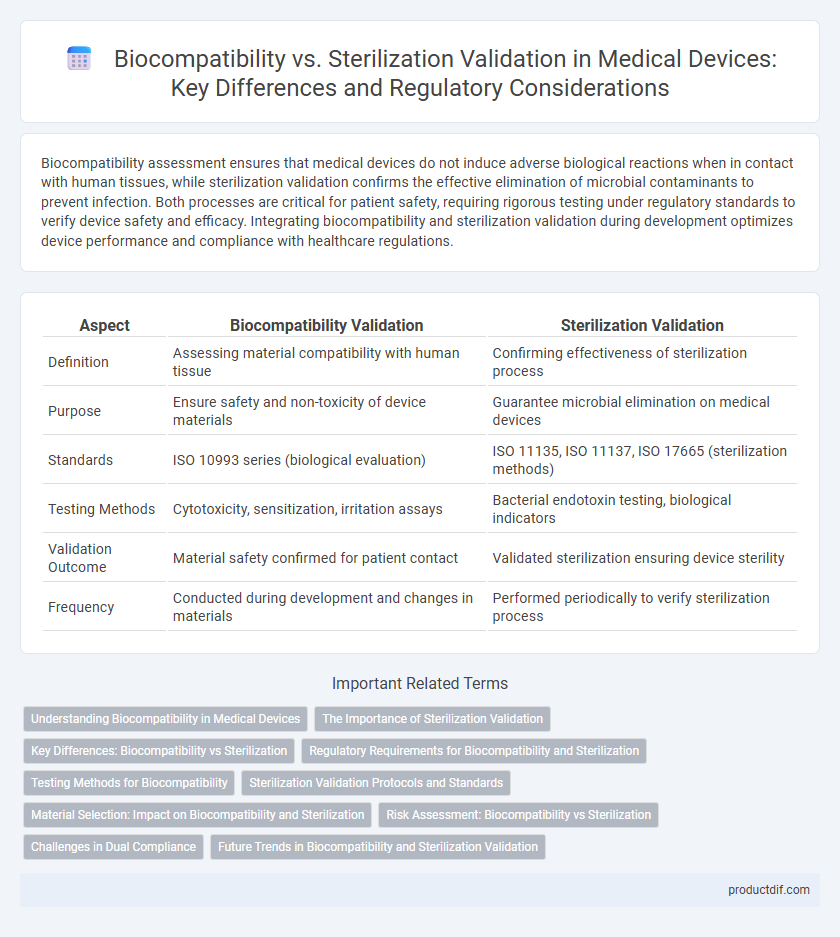
Biocompatibility assessment ensures that medical devices do not induce adverse biological reactions when in contact with human tissues, while sterilization validation confirms the effective elimination of microbial contaminants to prevent infection. Both processes are critical for patient safety, requiring rigorous testing under regulatory standards to verify device safety and efficacy. Integrating biocompatibility and sterilization validation during development optimizes device performance and compliance with healthcare regulations.
Table of Comparison
| Aspect | Biocompatibility Validation | Sterilization Validation |
|---|---|---|
| Definition | Assessing material compatibility with human tissue | Confirming effectiveness of sterilization process |
| Purpose | Ensure safety and non-toxicity of device materials | Guarantee microbial elimination on medical devices |
| Standards | ISO 10993 series (biological evaluation) | ISO 11135, ISO 11137, ISO 17665 (sterilization methods) |
| Testing Methods | Cytotoxicity, sensitization, irritation assays | Bacterial endotoxin testing, biological indicators |
| Validation Outcome | Material safety confirmed for patient contact | Validated sterilization ensuring device sterility |
| Frequency | Conducted during development and changes in materials | Performed periodically to verify sterilization process |
Understanding Biocompatibility in Medical Devices
Biocompatibility in medical devices ensures materials do not provoke adverse biological responses when in contact with patient tissues, crucial for device safety and efficacy. Thorough biocompatibility testing assesses cytotoxicity, sensitization, and irritation according to ISO 10993 standards, providing evidence for regulatory approval. Sterilization validation focuses on eliminating microbial contamination, but it must not compromise the biocompatibility or physical properties of the device materials.
The Importance of Sterilization Validation
Sterilization validation ensures that medical devices are free from viable microorganisms, maintaining patient safety and preventing infections during use. It involves rigorous testing of sterilization processes, including parameters like time, temperature, and chemical exposure, to confirm effectiveness and reproducibility. This validation is crucial for regulatory compliance and guarantees that biocompatibility is not compromised by residual contaminants or sterilization by-products.
Key Differences: Biocompatibility vs Sterilization
Biocompatibility validation ensures that medical devices do not cause adverse biological reactions when in contact with tissues or bodily fluids, focusing on cytotoxicity, sensitization, and irritation tests. Sterilization validation verifies the effectiveness of processes like steam, ethylene oxide, or radiation sterilization in eliminating microbial contaminants to achieve a specified sterility assurance level (SAL). The key difference lies in biocompatibility assessing safety related to human tissue interaction, while sterilization validation ensures microbial safety and infectivity control.
Regulatory Requirements for Biocompatibility and Sterilization
Regulatory requirements for biocompatibility validation in medical devices demand comprehensive testing according to ISO 10993 standards to ensure materials do not pose toxicological risks to patients. Sterilization validation must comply with ISO 11135, ISO 11137, or ISO 17665, depending on the sterilization method, ensuring effective microbial inactivation without compromising device integrity. Both processes require detailed documentation and risk assessment aligned with FDA and EU MDR guidelines to achieve regulatory approval.
Testing Methods for Biocompatibility
Testing methods for biocompatibility in medical devices primarily involve in vitro cytotoxicity assays, which assess cellular responses to material extracts, alongside in vivo tests like sensitization, irritation, and systemic toxicity evaluations according to ISO 10993 standards. Analytical techniques such as chemical characterization and endotoxin testing complement biological assays to ensure comprehensive evaluation of potential adverse effects. These methods differ fundamentally from sterilization validation, which focuses on microbial lethality using biological indicators and physical or chemical sterilization process controls.
Sterilization Validation Protocols and Standards
Sterilization validation protocols in medical device manufacturing are critical to ensure the elimination of microbial contamination while preserving device functionality and biocompatibility. These protocols adhere to standards such as ISO 11135 for ethylene oxide sterilization, ISO 11137 for radiation sterilization, and ISO 17665 for steam sterilization, providing comprehensive guidelines for process qualification, routine monitoring, and sterilization efficacy. Robust sterilization validation ensures compliance with regulatory requirements and patient safety by verifying sterilization processes through biological indicators, chemical indicators, and physical parameter controls.
Material Selection: Impact on Biocompatibility and Sterilization
Material selection critically influences both biocompatibility and sterilization validation in medical devices, as certain polymers and metals exhibit varying resistance to sterilization methods like steam autoclaving or ethylene oxide without compromising cellular compatibility. Biocompatible materials such as medical-grade silicone and titanium maintain integrity and minimize cytotoxicity after sterilization, ensuring patient safety and device efficacy. Rigorous testing aligned with ISO 10993 and ISO 11135 standards confirms that selected materials withstand sterilization cycles while preserving their biological performance.
Risk Assessment: Biocompatibility vs Sterilization
Risk assessment in medical device development critically evaluates biocompatibility and sterilization processes to ensure patient safety and regulatory compliance. Biocompatibility risk assessment focuses on potential toxicological and immunological responses from device materials, while sterilization risk assessment addresses microbial contamination and device integrity post-sterilization. Integrating these assessments helps identify potential failure modes, guiding the selection of materials and sterilization methods that minimize adverse effects and ensure overall device safety.
Challenges in Dual Compliance
Achieving dual compliance in biocompatibility and sterilization validation for medical devices presents challenges due to conflicting material and process requirements. Biocompatible materials may degrade or alter during sterilization, affecting device safety and efficacy. Ensuring validated sterilization methods do not compromise biocompatibility necessitates integrated testing protocols and close coordination between material science and sterilization engineering teams.
Future Trends in Biocompatibility and Sterilization Validation
Future trends in biocompatibility and sterilization validation for medical devices emphasize the integration of advanced in vitro models and computational simulations to predict biological responses more accurately, reducing reliance on animal testing. Emerging sterilization technologies like low-temperature plasma and vaporized hydrogen peroxide aim to enhance microbial inactivation while preserving device integrity and functionality. Regulatory bodies increasingly encourage the adoption of real-time monitoring systems and machine learning algorithms to optimize validation processes, ensuring higher safety standards and faster time-to-market.
Biocompatibility vs Sterilization validation Infographic
 productdif.com
productdif.com