Sterile medical devices undergo rigorous sterilization processes to eliminate all microorganisms, ensuring patient safety during invasive procedures. Non-sterile devices, while manufactured under controlled conditions, do not guarantee the complete absence of microbes and are typically used for external or non-invasive applications. Choosing between sterile and non-sterile devices depends on the intended use, with sterile options critical for surgeries and wound care to prevent infections.
Table of Comparison
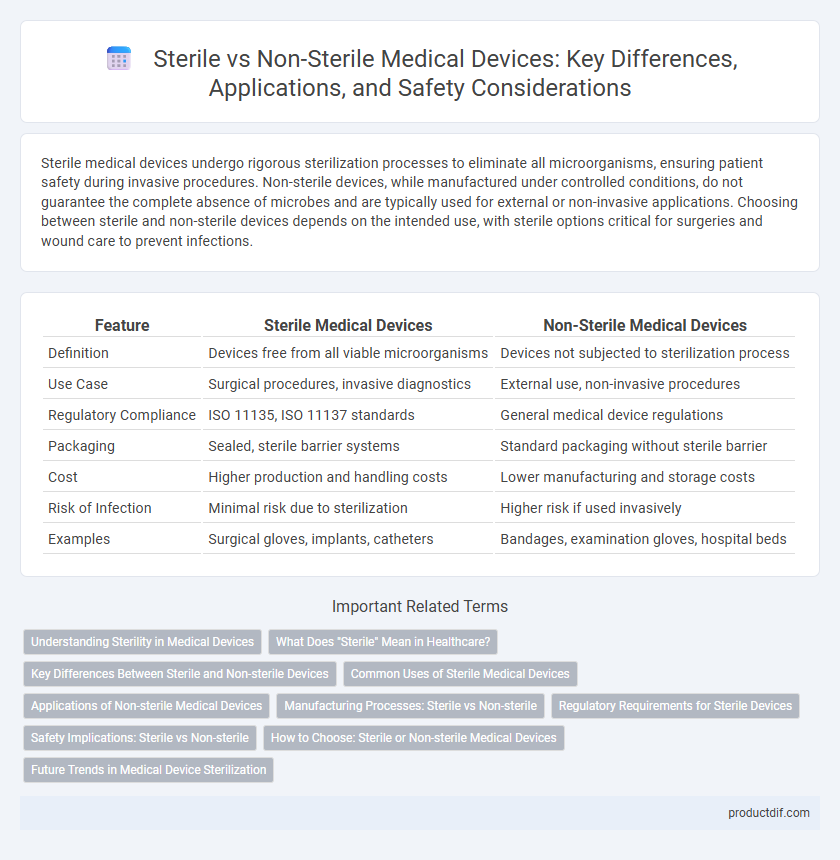
| Feature | Sterile Medical Devices | Non-Sterile Medical Devices |
|---|---|---|
| Definition | Devices free from all viable microorganisms | Devices not subjected to sterilization process |
| Use Case | Surgical procedures, invasive diagnostics | External use, non-invasive procedures |
| Regulatory Compliance | ISO 11135, ISO 11137 standards | General medical device regulations |
| Packaging | Sealed, sterile barrier systems | Standard packaging without sterile barrier |
| Cost | Higher production and handling costs | Lower manufacturing and storage costs |
| Risk of Infection | Minimal risk due to sterilization | Higher risk if used invasively |
| Examples | Surgical gloves, implants, catheters | Bandages, examination gloves, hospital beds |
Understanding Sterility in Medical Devices
Sterility in medical devices ensures the complete elimination of all viable microorganisms, crucial for preventing infections during surgical procedures or wound care. Sterile devices undergo rigorous sterilization processes such as autoclaving, ethylene oxide gas, or gamma irradiation, meeting strict regulatory standards like ISO 11135 and ISO 11737. Non-sterile devices, while not free from all microorganisms, are used in applications where sterility is not critical, emphasizing the importance of selecting the appropriate device type based on the intended clinical use.
What Does "Sterile" Mean in Healthcare?
Sterile in healthcare refers to the complete absence of all living microorganisms, including bacteria, viruses, fungi, and spores, achieved through processes like autoclaving, gamma radiation, or ethylene oxide sterilization. Sterile medical devices are crucial in invasive procedures to prevent infections and ensure patient safety, meeting stringent regulatory standards set by organizations such as the FDA and ISO 13485. Non-sterile devices, while manufactured in controlled environments, do not undergo sterilization and are typically used for external or non-invasive applications where microbial contamination poses less risk.
Key Differences Between Sterile and Non-sterile Devices
Sterile medical devices are free from all viable microorganisms, achieved through processes like autoclaving or gamma irradiation, ensuring safety for invasive procedures. Non-sterile devices do not undergo these sterilization processes and are suitable for external or non-invasive applications, carrying a higher risk of contamination. The choice between sterile and non-sterile devices depends on the intended use, regulatory standards, and patient safety requirements.
Common Uses of Sterile Medical Devices
Sterile medical devices are primarily used in surgical procedures, invasive diagnostic tests, and wound care to minimize the risk of infection and ensure patient safety. Common examples include surgical instruments, catheters, implants, and syringes, all of which require strict sterilization protocols. Their usage is critical in hospital settings, outpatient clinics, and emergency care to maintain aseptic conditions and prevent microbial contamination.
Applications of Non-sterile Medical Devices
Non-sterile medical devices are primarily used in non-invasive procedures such as physical examinations, diagnostic testing, and external patient monitoring. These devices include items like blood pressure cuffs, stethoscopes, and crutches, which do not require sterilization due to limited contact with sterile tissue or the bloodstream. Non-sterile devices play a critical role in routine patient care and diagnostics by minimizing infection risk while offering cost-effective and reusable solutions.
Manufacturing Processes: Sterile vs Non-sterile
Manufacturing processes for sterile medical devices involve aseptic techniques, terminal sterilization methods like gamma irradiation or ethylene oxide, and strict environmental controls to prevent contamination. Non-sterile device production emphasizes cleanliness and material biocompatibility without the need for sterilization validation or cleanroom standards. Regulatory requirements such as ISO 13485 and FDA guidance dictate specific process controls and documentation for sterile device manufacturing to ensure patient safety and product efficacy.
Regulatory Requirements for Sterile Devices
Regulatory requirements for sterile medical devices mandate stringent compliance with sterilization standards such as ISO 11135 and ISO 11737, ensuring products are free from viable microorganisms. Manufacturers must validate sterilization processes through documented evidence, including bioburden testing and sterility assurance levels (SAL), to satisfy authorities like the FDA and EMA. Labeling and packaging also require strict controls to maintain sterility until point of use, supporting patient safety and regulatory approvals.
Safety Implications: Sterile vs Non-sterile
Sterile medical devices eliminate microbial contamination, significantly reducing the risk of infections during surgical and invasive procedures, which is critical for patient safety and compliance with regulatory standards like ISO 11737. Non-sterile devices may pose higher risks of introducing pathogens, necessitating stringent handling protocols and usage limitations, particularly in immunocompromised patients. Proper sterilization validation and packaging integrity assessments are essential to ensure device safety and minimize postoperative complications.
How to Choose: Sterile or Non-sterile Medical Devices
Choosing sterile or non-sterile medical devices depends on the procedure's risk level and infection control requirements; sterile devices are essential for invasive surgeries and wound care to prevent infection. Non-sterile devices can be used in procedures with minimal infection risk or for external applications where sterility is not critical. Assessing patient safety, device usage, and regulatory guidelines ensures optimal selection between sterile and non-sterile options.
Future Trends in Medical Device Sterilization
Emerging sterilization technologies, such as low-temperature plasma and vaporized hydrogen peroxide, are revolutionizing medical device sterilization by offering enhanced microbial control without compromising device integrity. Integration of IoT-enabled sterilization tracking systems facilitates real-time monitoring and ensures compliance with stringent regulatory standards such as ISO 13485. Advances in biodegradable sterilization packaging materials also align with sustainable healthcare initiatives, reducing environmental impact while maintaining sterility assurance levels.
Sterile vs Non-sterile Infographic
 productdif.com
productdif.com