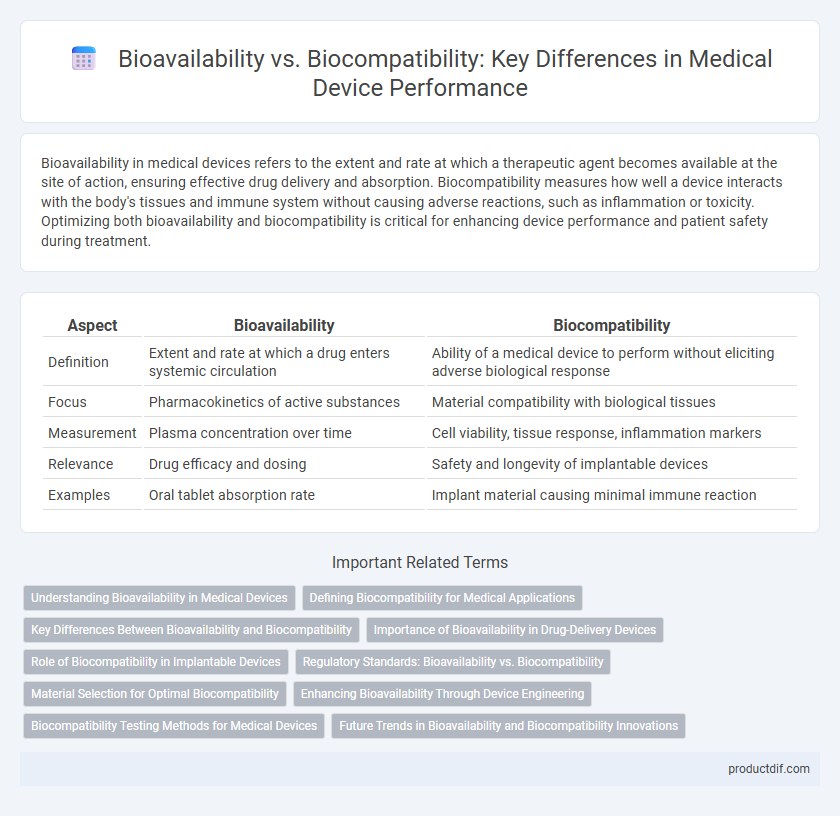
Bioavailability in medical devices refers to the extent and rate at which a therapeutic agent becomes available at the site of action, ensuring effective drug delivery and absorption. Biocompatibility measures how well a device interacts with the body's tissues and immune system without causing adverse reactions, such as inflammation or toxicity. Optimizing both bioavailability and biocompatibility is critical for enhancing device performance and patient safety during treatment.
Table of Comparison
| Aspect | Bioavailability | Biocompatibility |
|---|---|---|
| Definition | Extent and rate at which a drug enters systemic circulation | Ability of a medical device to perform without eliciting adverse biological response |
| Focus | Pharmacokinetics of active substances | Material compatibility with biological tissues |
| Measurement | Plasma concentration over time | Cell viability, tissue response, inflammation markers |
| Relevance | Drug efficacy and dosing | Safety and longevity of implantable devices |
| Examples | Oral tablet absorption rate | Implant material causing minimal immune reaction |
Understanding Bioavailability in Medical Devices
Bioavailability in medical devices refers to the proportion of a drug or therapeutic agent released from the device that becomes accessible at the target site for therapeutic effect, directly impacting treatment efficacy. It is critical to differentiate bioavailability from biocompatibility, which pertains to the device's ability to perform without eliciting adverse biological responses. Optimizing bioavailability ensures precise drug delivery and maximizes clinical outcomes in implantable and transdermal medical devices.
Defining Biocompatibility for Medical Applications
Biocompatibility in medical devices refers to the ability of a material to perform with an appropriate host response when applied within the body, minimizing adverse reactions such as inflammation or toxicity. Unlike bioavailability, which measures the extent and rate at which a drug reaches systemic circulation, biocompatibility focuses on ensuring the material's safety and functionality in direct contact with biological tissues. Key parameters for defining biocompatibility include cytotoxicity, sensitization, irritation, and long-term stability within physiological environments.
Key Differences Between Bioavailability and Biocompatibility
Bioavailability measures the extent and rate at which an active pharmaceutical ingredient or drug is absorbed and becomes available at the site of physiological activity, crucial for drug efficacy. Biocompatibility refers to the compatibility of a medical device or material with living tissue, ensuring it does not provoke an immune response or toxicity when implanted or in contact with the body. The key difference lies in bioavailability focusing on drug absorption and therapeutic effect, while biocompatibility emphasizes the safety and tolerance of materials within biological systems.
Importance of Bioavailability in Drug-Delivery Devices
Bioavailability in drug-delivery devices determines the extent and rate at which the active pharmaceutical ingredient enters systemic circulation, directly impacting therapeutic effectiveness. High bioavailability ensures optimal drug concentration at the target site, enhancing treatment outcomes and minimizing dosage frequency. This contrasts with biocompatibility, which primarily addresses the device's compatibility with biological tissues, making bioavailability a critical factor in the design of effective medical drug-delivery systems.
Role of Biocompatibility in Implantable Devices
Biocompatibility in implantable medical devices ensures that materials do not elicit adverse immune responses, fostering tissue integration and long-term functionality. This property is critical for maintaining device stability and preventing inflammation or rejection in the human body. Unlike bioavailability, which measures the extent of drug absorption, biocompatibility focuses on the safe interaction between device materials and biological tissues.
Regulatory Standards: Bioavailability vs. Biocompatibility
Regulatory standards for medical devices require clear differentiation between bioavailability and biocompatibility to ensure safety and efficacy. Bioavailability standards focus on the rate and extent of active substance absorption, critical for drug-delivery devices, while biocompatibility standards evaluate material interactions with biological systems, guided by ISO 10993 series. Compliance with FDA and EMA regulations mandates rigorous testing protocols addressing both bioavailability parameters and biocompatibility assessments to meet approval criteria.
Material Selection for Optimal Biocompatibility
Material selection for optimal biocompatibility in medical devices requires evaluating the interaction between device materials and biological systems to minimize adverse immune responses. High bioavailability ensures active compounds or therapeutic agents are effectively delivered at target sites, while biocompatibility guarantees the material does not provoke toxicity or inflammation. Advanced polymers, ceramics, and titanium alloys are commonly chosen for their proven biocompatibility and ability to maintain functional bioavailability in implantable devices.
Enhancing Bioavailability Through Device Engineering
Enhancing bioavailability through medical device engineering involves optimizing drug delivery systems to improve the absorption and therapeutic effect of active pharmaceutical ingredients. Innovations such as nano-structured coatings, controlled release mechanisms, and targeted delivery platforms significantly increase drug bioavailability while maintaining biocompatibility to ensure minimal tissue reaction and long-term safety. Advanced materials and surface modifications in implantable devices are critical for achieving precise drug release profiles and reducing systemic side effects.
Biocompatibility Testing Methods for Medical Devices
Biocompatibility testing methods for medical devices include cytotoxicity, sensitization, and irritation tests to evaluate tissue compatibility and potential immune responses. In vitro assays assess cellular responses, while in vivo tests like implantation and systemic toxicity studies analyze long-term effects on living organisms. These methods ensure material safety and regulatory compliance, minimizing adverse reactions during clinical use.
Future Trends in Bioavailability and Biocompatibility Innovations
Future trends in bioavailability emphasize advanced drug delivery systems using nanotechnology and targeted release mechanisms to enhance therapeutic efficacy and reduce side effects. Innovations in biocompatibility focus on smart biomaterials with self-healing properties and real-time monitoring interfaces to improve device integration and patient safety. Integration of artificial intelligence and machine learning accelerates the design of personalized medical devices ensuring optimal bioavailability and biocompatibility.
Bioavailability vs Biocompatibility Infographic
 productdif.com
productdif.com